Given the well-known health harms of smoking, tobacco is regulated and taxed nearly everywhere in the world. With the introduction of electronic nicotine delivery systems (ENDS), commonly known as e-cigarettes, new questions have arisen about the risks to health from their use and whether they should be regulated as strictly as tobacco. In some quarters, the possibility that e-cigarettes and vaping could deliver an attractive, smoking-like sensory experience while avoiding the health harms that accompany combusting and inhaling tobacco has been greeted with enthusiasm, since the new products could help some smokers transition to a less risky product. In other quarters, and in much of the American public health community, e-cigarettes were greeted with skepticism and hostility, since they could potentially renormalize smoking, set back the great gains in tobacco control of the past several decades, and hook a new generation of young people on nicotine and smoking. This chapter covers the regulatory history of tobacco and e-cigarettes, summarizes upcoming regulatory actions and challenges, discusses the key issues involved in the regulation of these activities, and includes suggestions for better regulation.
Readers will benefit from an understanding of some vaping technology and terminology. All e-cigarettes work by means of a battery-operated heater that vaporizes a solution containing nicotine and flavoring (known as an eliquid), which is then inhaled by the user. Sometimes grouped with e-cigarettes are heat-not-burn products that heat ground tobacco without combustion. There are many types of e-cigarettes and vaping systems, from cartridge-based “closed” systems, in which the consumer buys a disposable, unmodifiable eliquid cartridge, to tank-based “open” systems, in which the vaper buys vials of eliquid for refill and can customize what is vaped. All of these will be referred to as “e-cigarettes” in this chapter, and their consumption will be called “vaping,” unless a distinction among products is required. The exception is that discussions of the scientific literature on the health effects of e-cigarettes exclude heat-not-burn products, which are typically not included in the studies. Finally, note that using e-cigarettes is not “smoking”—nothing is combusted and there is no smoke.
History of Tobacco Regulation in the United States
From 1900 to 1963, per capita consumption of cigarettes grew rapidly, from a low figure in 1900 until in the latter year the daily average was more than half a pack per adult.1Institute of Medicine, Ending the Tobacco Problem: A Blueprint for the Nation, ed. Richard J. Bonnie, Kathleen Stratton, and Robert B. Wallace (Washington, DC: National Academies Press, 2007). The watershed moment in the history of smoking in the United States was the publication of the Surgeon General’s report in 1964, which stated that “cigarette smoking is a health hazard of sufficient importance in the United States to warrant appropriate remedial action.”2US Department of Health, Education, and Welfare, Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service (Washington, DC: US Government Printing Office, 1964), 32. After that year, consumption began its long decline, falling to 0.13 packs sold a day per adult in 2018.3Euromonitor International, Tobacco in the United States, Country Report, January 2019, Passport.
Of course, the average smoker consumes more than that. In 2018, adult smokers reported smoking a bit more than half a pack a day, while retail sales of cigarettes averaged a bit less than one pack per day per adult smoker.4The smoking intensity figure of 11.5 cigarettes per day (with a 95% confidence interval for the mean of [11.2, 11.8]) is calculated by the author from the 2018 Tobacco Use Supplement to the Current Population Survey. The retail sales figures are from Euromonitor International, Tobacco in the United States. The discrepancy between self-reported smoking behavior and sales per adult smoker is due to the well-known fact that survey respondents tend to underreport smoking and to the fact that many underage smokers consume some of the sales. That same year, there were about 34 million adult cigarette smokers in the US and 49 million adult users of any tobacco product, including e-cigarettes.5MeLisa R. Creamer et al., “Tobacco Product Use and Cessation Indicators among Adults—United States, 2018,” Morbidity and Mortality Weekly Report 68, no. 45 (2019): 1013–19. These figures imply that the prevalence of cigarette smoking has fallen to 13.7 percent among US adults, while the prevalence of any form of tobacco consumption is 19.7 percent. Adult cigarette smoking prevalence has declined about two-thirds from its peak in the 1960s.
The sale and use of tobacco in the US has been regulated in various ways for decades, although much of the regulatory action has come relatively recently compared to the long history of smoking. The first federal action regarding the tobacco industry and the health effects of its products was the requirement that cigarette manufacturers add the notice that smoking “may be hazardous to your health” on packs. The health warning, which came into effect in 1966, was the first of its kind in the world.6Heikki Hiilamo, Eric Crosbie, and Stanton A. Glantz, “The Evolution of Health Warning Labels on Cigarette Packs: The Role of Precedents, and Tobacco Industry Strategies to Block Diffusion,” Tobacco Control 23, no. 1 (2014): e2.
Despite the landmark surgeon general’s report in 1964, until the 1980s tobacco was specifically exempted from legislation (e.g., the Toxic Substances Control Act) and regulation (e.g., by the Consumer Product Safety Commission) that otherwise would have curtailed the industry or the freedom to smoke.7Institute of Medicine, Ending the Tobacco Problem. Starting in 1985, a set of four rotating health warnings with stronger wording were required on cigarette packaging.8Hiilamo, Crosbie, and Glantz, “Evolution of Health Warning Labels.” The FDA sought to add graphical health warnings in 2011, but legal action by the tobacco industry has delayed the requirement for almost a decade.9See Tobacco Products; Required Warnings for Cigarette Packages and Advertisements, 84 Fed. Reg. 42754 (August 16, 2019), and the discussion below.
The first federally mandated restrictions on where one could smoke came in the late 1980s, with bans on smoking on certain domestic airline flights.10Pub. L. No. 100-202 (1987) banned smoking on domestic airline flights scheduled for two hours or less, while Pub. L. No. 101-164 (1989) did the same for flights scheduled for six hours or less. The so-called Synar Amendment of 1992 required all states to adopt and enforce restrictions on the sales and distribution of tobacco to minors; federal enforcement of the restrictions (through the withholding of certain federal payments to the states) went into effect in 1996.11States were required to have (and enforce through random inspections) laws “prohibiting any manufacturer, retailer or distributor of tobacco products from selling or distributing such products to any individual under the age of 18.” In the event of noncompliance, a state would lose eligibility for a Substance Abuse Prevention and Treatment Block Grant. See Tobacco Regulation for Substance Abuse Prevention and Treatment Block Grants, 61 Fed. Reg. 1492 (January 19, 1996). While as recently as the 1980s some states had no restrictions on sales to minors, however defined, by 1995 all states and the District of Columbia prohibited the sale and distribution of tobacco products to those under 18 years of age.12See Dorie E. Apollonio and Stanton A. Glantz, “Minimum Ages of Legal Access for Tobacco in the United States from 1863 to 2015,” American Journal of Public Health 106, no. 7 (2016): 1200–207; and D. M. Shelton et al., “State Laws on Tobacco Control—United States, 1995,” Morbidity and Mortality Weekly Report Surveillance Summaries 44, no. 6 (1995): 1–28.
In 1998, the three major tobacco manufacturers signed the Master Settlement Agreement (MSA) with 46 states. In exchange for immunity from legal claims by these states for costs incurred for smoking-related illnesses and deaths, the three major tobacco manufacturers agreed to pay the states an estimated $206 billion, finance a $1.5 billion anti-smoking campaign, and cease various forms of advertising, product placement, and event sponsorship, as well as any form of marketing aimed at youth. While the settling states say that “the central purpose of the MSA is to reduce smoking, especially in American youth,”13The statement is from the National Association of Attorneys General Center for Tobacco and Public Health, the organization set up by the attorneys general of the settling states to handle matters pertaining to the MSA. See “NAAG Center for Tobacco and Public Health,” National Association of Attorneys General, accessed July 2, 2020, https://www.naag.org/naag/about_naag/naag-center-for-tobacco-and-public-health.php. it appears that the states spend little of the money collected from the MSA and tobacco taxes on tobacco prevention and cessation programs—well under 3 percent of it in 2020.14“A State-by-State Look at the 1998 Tobacco Settlement 21 Years Later,” Campaign for Tobacco-Free Kids, last modified January 16, 2020, https://www.tobaccofreekids.org/what-we-do/us/statereport.
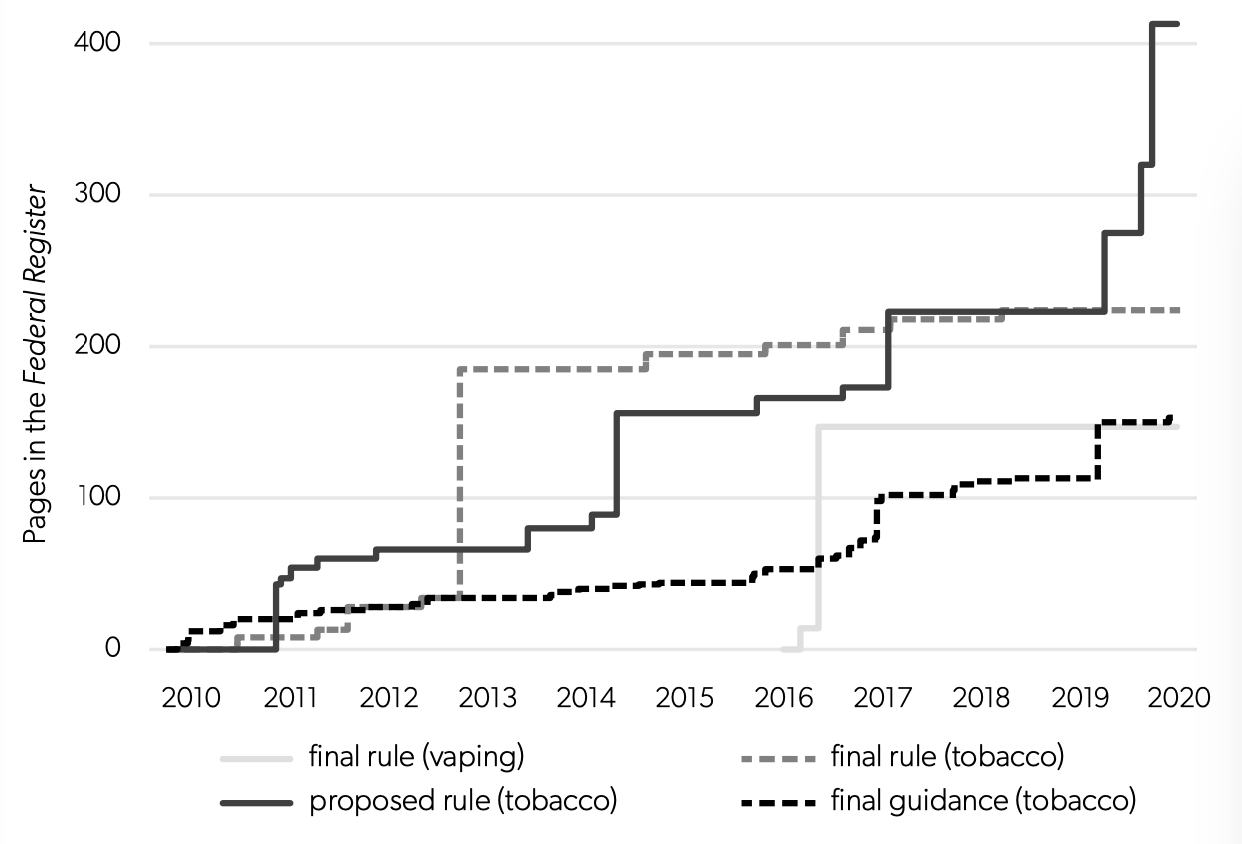
The entering wedge for direct federal regulation of tobacco as a consumer product came in the form of Family Smoking Prevention and Tobacco Control Act of 2009, which granted the FDA authority to regulate tobacco products. The FDA’s first action under the act was to issue a rule in 2010 prohibiting the sale of cigarettes and smokeless tobacco to any person under age 18. (Such sales were already illegal in all states.)15See Regulations Restricting the Sale and Distribution of Cigarettes and Smokeless Tobacco to Protect Children and Adolescents, 75 Fed. Reg. 13225 (March 19, 2010). The rule was a revised version of a 1996 FDA rule that was ultimately voided by the Supreme Court, which ruled in 2000 that the FDA lacked the authority to regulate tobacco as a drug. FDA v. Brown & Williamson Tobacco Corp. (98-1152), 529 U.S. 120 (2000), 153 F.3d 155, affirmed. Since that time, there has been a steady flow of proposed and final rules and “guidance” from the FDA regarding tobacco regulation. Figure 1 shows the growth of federal regulation regarding tobacco over time, as measured by the cumulative number of pages of rules in the Federal Register. By 2015, there were over 200 pages of binding regulations, and by the beginning of 2020 there were 224 pages of rules, more than 150 pages of guidance regarding those rules, and well over 400 accumulated pages of proposed rules. The pages of proposed rules nearly doubled in 2019 with recent actions by the FDA (about which more will be said below).
In the first of two recent federal regulatory actions, the age threshold for retail sales of tobacco products after December 2019 was raised from 18 to 21 years.16The new regulation (which took effect immediately when President Trump signed the bill on December 20, 2019) amends the Federal Food, Drug, and Cosmetics Act at 21 U.S.C. 387f(d) to include the higher minimum age of retail sale for any tobacco product, including ecigarettes (because of the FDA deeming action described in the next section). Before that time, well fewer than half the states had an age restriction that high. In its most recent action, the FDA issued rules requiring graphical warnings on cigarette packages.17Tobacco Products; Required Warnings for Cigarette Packages and Advertisements, 84 Fed. Reg. 42754 (August 16, 2019). These new color graphics depicting the negative health consequences of smoking will occupy the entire top half of the area of the front and rear faces of cigarette packages.18For the final rule, see Tobacco Products; Required Warnings for Cigarette Packages and Advertisements, 85 Fed. Reg. 15638 (March 18, 2020). Some research indicates that such large graphical warnings are more likely to be noticed by smokers or more likely to lead them to consider cessation or smoking less.19See David Hammond et al., “Text and Graphic Warnings on Cigarette Packages: Findings from the International Tobacco Control Four Country Study,” American Journal of Preventive Medicine 32, no. 3 (2007): 202–9; Seth M. Noar et al., “Pictorial Cigarette Pack Warnings: A Meta-analysis of Experimental Studies,” Tobacco Control 25, no. 3 (2016): 341–54. However, apparently no study has shown that graphical warnings lead to an increase in actual cessation (versus stated intentions to quit).
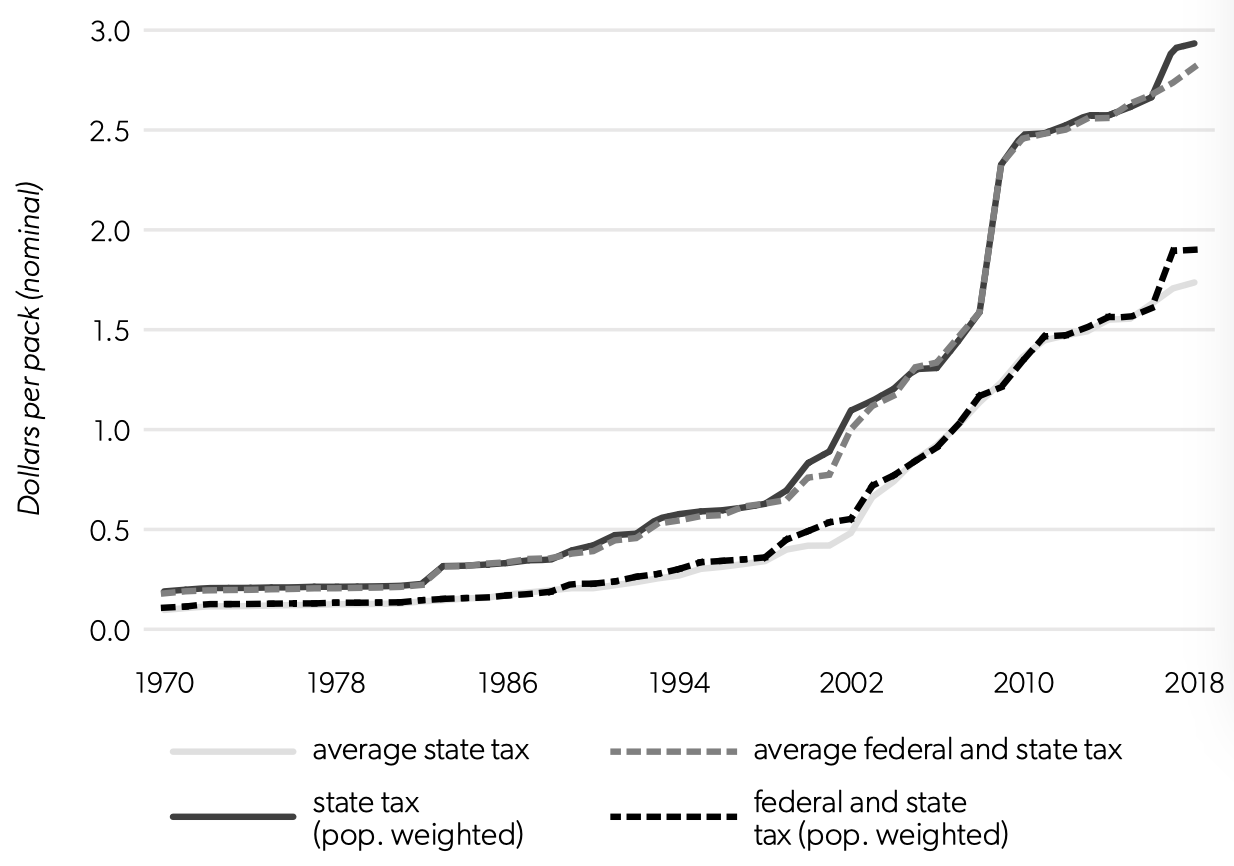
In addition to tobacco regulations, the federal government has levied excise taxes on cigarettes continuously since the time of the Civil War.20The Tax Burden on Tobacco: Historical Compilation (Arlington, VA: Orzechowski and Walker, 2014). The tax remained at 8 cents a pack from 1951 until 1983, when it was doubled. In the early 1990s the tax was raised to 24 cents, and in the early 2000s it was raised by stages to 39 cents. In 2009, the largest increase yet resulted in a per-pack federal tax of $1.01, where it remains in 2020.
Figure 1. Growth of Federal Regulation from the FDA Regarding Tobacco and E-cigarettes
Source: Author’s calculations from FDA data, https://www.fda.gov/media/88873/download.
State taxes on tobacco vary widely, although most states have increased their cigarette taxes in the past two decades. From 1970 to 2018, the average state excise tax (not weighted for population or consumption) increased from 9.6 cents per pack to $1.74—an annualized nominal growth rate of 7.5 percent and an inflation-adjusted growth rate of 3.6 percent (see figure 2). State taxes grew exceptionally quickly after 2000, with an inflation-adjusted growth rate of the average tax of 5.5 percent per year. Adding the federal tax on top of the state taxes shows that the combined nominal rates rose by an average of 5.7 percent per year between 1970 and 2018 and have risen by 6.9 percent per year since 2000. These large increases in the taxes over time resulted in almost 40 percent of the retail sales prices of cigarettes going to excise taxes in 2018—or, to put it another way, an effective 65 percent tax rate on a pack.
Figure 2 also shows the population-weighted averages of the taxes; these reflect the excise taxes facing the average person in the nation. For the most part these are similar to the simple averages, with the exception of a divergence in 2017 owing to California enacting a large tax increase. Overall, these levels of taxation make cigarettes one of the most highly taxed products in the nation. By comparison, state alcohol taxes averaged only three to five cents per drink in 2015.21See Timothy S. Naimi et al., “Erosion of State Alcohol Excise Taxes in the United States,” Journal of Studies on Alcohol and Drugs 79, no. 1 (2018): 43–48.
History of E-cigarette Regulation in the United States
The market for e-cigarette products in the United States began to take off around 2006. In 2008, the e-cigarette market had only $28 million in revenue from an estimated 190,000 vapers, but by 2017 it was a $4.6 billion market with an estimated 8.4 million vapers.22Euromonitor International, Tobacco in the United States. Those figures represent a revenue growth rate of over 50 percent per year. Given the recent emergence of e-cigarettes as a significant product, it is unsurprising that the regulatory history of vaping is short. In 2016, the FDA “deemed” e-cigarettes (or, more properly speaking, ENDS) to be tobacco products.23Ned Sharpless, “How FDA is Regulating E-Cigarettes,” September 10, 2019, https://www.fda.gov/news-events/fda-voices/how-fda-regulating-e-cigarettes.
Figure 2. Growth of State and Federal Excise Taxation on Cigarettes
Source: Data from the Centers for Disease Control and Prevention, “Tax Burden on Tobacco, 1970-2018,” August 13, 2020, https://chronicdata.cdc.gov/Policy/The-Tax-Burden-on-Tobacco-1970-2018/7nwe-3aj9.
While the FDA has the legal authority to deem new or existing products to be tobacco products, and thus subject to its regulatory authority, it is worth noting that ENDS do not contain tobacco. While nicotine is the addictive substance found in tobacco, it is the other constituents in tobacco that, when combusted and inhaled, cause the main health problems associated with smoking. In particular, to quote a report from the National Academies of Sciences, Engineering, and Medicine, “There is no evidence to indicate that nicotine is a carcinogen.”24National Academies of Sciences, Engineering, and Medicine, Public Health Consequences of Ecigarettes (Washington, DC: National Academies Press, 2018). Thinking of e-cigarettes as tobacco products thus greatly confuses the issue, a point to which I will return below.
After deeming e-cigarettes to be tobacco products, the FDA aimed its entire set of tobacco-related regulations at vaping products as well. Manufacturers of existing products had to register with the FDA and submit lists of products, their ingredients, and evidence about their health effects.25See the review of the regulatory status of ecigarettes provided by the Ned Sharpless, the acting commissioner of the FDA. Ned Sharpless, “How FDA Is Regulating Ecigarettes,” Food and Drug Administration, September 10, 2019, https://www.fda.gov/news-events/fda-voices-perspectives-fda-leadership-and-experts/how-fda-regulating-e-cigarettes. Manufacturers are now required to place on product packaging a warning that they contain nicotine and that nicotine is an addictive chemical. Products introduced between 2007 and August 2016 could continue to be sold while their applications for regulatory approval were considered by the FDA.26After a court decision, the deadline for filing the applications with the FDA was initially set at May 12, 2020, but this was later extended by 120 days because of impacts from COVID-19 in April. The court ordered that products with timely applications could remain on the market for one year pending FDA review. New e-cigarette products are not allowed to be introduced after August 2016 without premarket approval. Since the FDA has not ruled on any e-cigarette application yet, in part because continuing legal action made uncertain the deadline for submission of applications, anti-vaping advocates can still truthfully claim that there are no FDA-approved e-cigarettes on the market.27The one partial exception is Philip Morris International’s heat-not-burn product IQOS, which heats tobacco (unlike conventional ENDS, which vaporize an eliquid) without combustion so that the vapor can be inhaled. Heat-not-burn products are often considered a different category from ecigarettes by users, researchers, and manufacturers. In January 2020, the FDA also effectively prohibited sales of flavored cartridge-based e-cigarettes (other than tobacco-, mint-, and menthol-flavored e-cigarettes).28See Food and Drug Administration, Enforcement Priorities for Electronic Nicotine Delivery Systems (ENDS) and Other Deemed Products on the Market without Premarket Authorization: Guidance for Industry, January 2020, https://www.fda.gov/media/133880/download. However, flavored eliquids for open-system tank vaping (typically available at vape shops) remain allowed.29More properly speaking, they are technically still illegal (as with all ENDS apart from IQOS), but are not candidates for FDA enforcement at the present time.
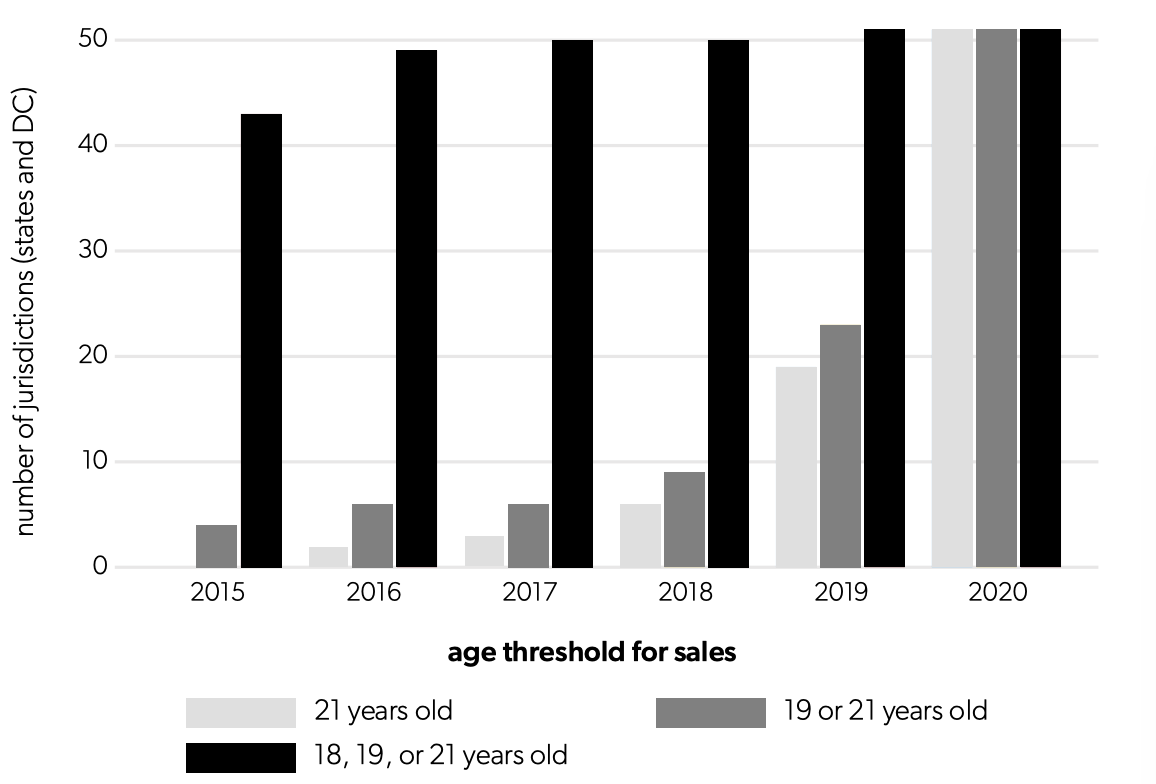
With e-cigarettes added to the regulatory purview of the FDA, age restrictions on sales to youth under age 18 and the prohibition of sales from vending machines came into force in 2016.30However, as discussed in note 11 above, rather than functioning as an outright restriction, the federal age limit is instead enforced through financial consequences for states that do not so restrict sales. As figure 3 shows, nearly all states followed the FDA’s prompting. Michigan, however, did not restrict sales of ecigarettes to minors until April 2019. See Malachi Barrett, “Michigan Senate Approves Ban on Ecigarette Sales to Minors,” MLive, April 23, 2019. Most states had already banned sales to youth before the federal action (see figure 3), and over time many states raised their age restrictions on sales to 19 or 21 years. Near the end of 2019, as mentioned above, the federal age limit was raised to 21 for all tobacco products, including e-cigarettes.
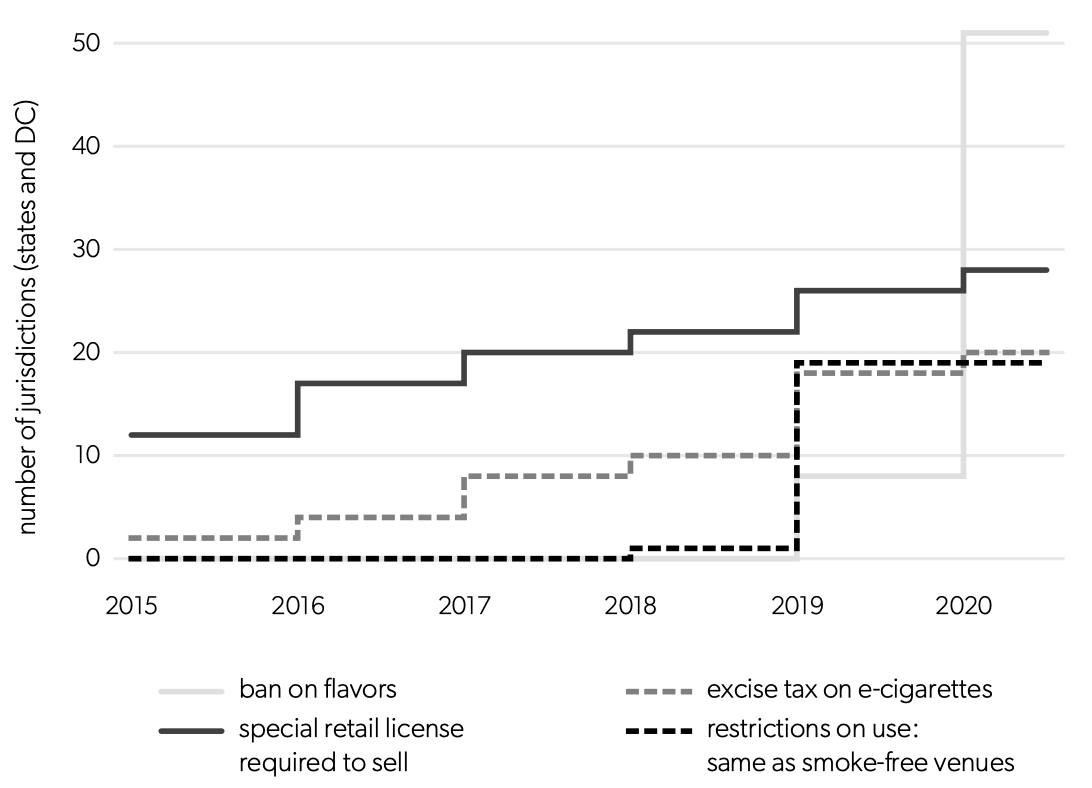
States have also been free to impose other regulation on the sales and usage of e-cigarettes. The increasing number of other regulations among the states is depicted in figure 4. Some states require retailers to obtain special licenses to sell e-cigarettes, typically with the goal of limiting youth access to vaping products; some place the same restrictions on vapers regarding using the devices in public as on smokers (thus applying “smoke-free” rules to a smoke-free product). Finally, a minority of states levy excise taxes on e-cigarettes (in contrast to ubiquitous state taxes on cigarettes).
Upcoming Potential Regulatory Changes
The FDA is currently undertaking several rulemaking processes on tobacco regulation. One regulatory proceeding is considering whether menthol flavoring in cigarettes will be banned (other flavors are already illegal).31For the advance notice of proposed rulemaking, see 83 Fed. Reg. 12294 (March 21, 2018). The due date for comments from interested parties was extended to July; see 83 Fed. Reg. 26618 (June 8, 2018). Perhaps the most ambitious regulatory action contemplated by the FDA is to lower the nicotine content in cigarettes to minimally addictive or nonaddictive levels.32For the advance notice of proposed rulemaking, see 83 Fed. Reg. 11818 (March 16, 2018). While the FDA does not have the authority to ban cigarettes outright, such action would effectively kill the legal market for the product as it exists today. Public comments on the latter two proceedings were due in the summer of 2018, but the FDA has not issued final rules for either (or announced that it is abandoning the effort) as of the start of 2020.
As discussed earlier, apart from a single heat-not-burn product, the FDA has not issued rulings on any of the submissions for regulatory product approval for e-cigarette products. Thus, the industry faces a large degree of uncertainty going forward regarding the amount of effort required for successful submissions. The fact that the one approved product, IQOS by Philip Morris International, purportedly required billions of dollars for regulatory compliance on the part of the manufacturer and experienced two years of regulatory delay until approval does not bode well for any maker of e-cigarettes, apart from the largest tobacco manufacturers.33For the rough cost estimate, see Jennifer Maloney, “FDA Clears Philip Morris International Heat-Not-Burn IQOS Device for Sale in U.S.,” Wall Street Journal, April 30, 2019.
The main upcoming regulatory action by the FDA—eagerly awaited by industry and the public health community—is not new regulation per se, but rather a definitive ruling on any of the regulatory approvals sought for e-cigarette products (discussed above). It remains to be seen whether any such products will be allowed to claim that they are safer than cigarettes or that they aid in cessation of smoking. It is also unclear whether any cartridge-based ENDS flavored with something other than mint or menthol will be approved; despite the current sales ban, the FDA has not ruled out granting regulatory approval for such products. As mentioned above, the only ruling to date has been on a heat-not-burn product, which differs in many ways from traditional vaping products.
Figure 3. Growth of State Regulation Regarding E-cigarette Sales to Youth
Sources: Tobacco Control Legal Consortium, U.S. E-cigarette regulation: a 50-state review, 2020. Available from https://publichealthlawcenter.org/resources/us-e-cigarette-regulations-50-state-review.
Figure 4. Growth of State Regulations Regarding E-cigarette Sales and Usage
Sources: Public Health Law Center, “E-Cigarette Tax : States with Laws Taxing E-Cigarettes,” 2020; Public Health Law Center, Retail Licensure on E-Cigarettes: States with Laws Requiring Licenses for Retail Sales of E-Cigarettes, 2020; Public Health Law Center, “U.S. E-Cigarette Regulation: A 50-State Review.”
Issues Involved with Taxing and Regulating Tobacco
This section covers the various rationales offered for regulating tobacco and some of the unintended consequences of doing so. The three main rationales for excise taxes and regulations on tobacco fall into two categories. The main economic rationale has traditionally been to tax tobacco to align the private and social costs of smoking. The main actual rationale appears to be paternalism. In recent years, a hybrid rationale has emerged in which theories from behavioral economics are used to justify paternalistic taxation and regulation. These rationales are all discussed here.
The economic rationale for regulation: externalities.
The traditional economic rationale for tobacco taxation is that it serves to correct consumers’ faulty incentives (i.e., it is taxation to correct for externalities, à la economist Arthur C. Pigou). In other words, the main economic rationale for tobacco taxation depends on the presence of negative externalities.
An externality in this context is an effect of consumption that creates adverse consequences for persons other than the decision maker. So-called Pigovian taxes are set to correct for the externalities, so that consumers consider the costs and benefits of their actions from the social rather than merely the personal perspective. The two externalities discussed for consumption of tobacco are the burdens imposed on taxpayers (fiscal externalities) and the burdens imposed on nonsmokers (health externalities).34The discussion here follows Kenneth Warner et al., “Criteria for Determining an Optimal Cigarette Tax: The Economist’s Perspective,” Tobacco Control 4, no. 4 (1995): 380–86. When smokers degrade their likely future health by their consumption of tobacco, they create future expected costs for publicly funded health programs such as Medicare. However, whether it is proper to treat such “fiscal externalities” identically to other externalities in the social calculus is debated.35The argument presented here is from Edgar K. Browning, “The Myth of Fiscal Externalities,” Public Finance Review 27, no. 1 (January 1999): 3–18. Externalities require attention and possibly correction because they create inefficiencies, not because they transfer benefits from one party to another in the economy. The inefficiencies associated with fiscal externalities, however, are due to the inefficiencies inherent in subsidized healthcare, not to smoking per se. That is, the inefficiency (if any) arises because of the policy (Medicare), not the individual’s action (smoking).
The remaining difficulties with an argument based on fiscal externalities, for those wishing to justify high tax rates on cigarettes, are twofold. First, the cost of a pack is borne today (by the buyer), but any external costs for society to fund healthcare are far in the future. The present expected discounted value of those future healthcare costs is small, and thus so would be the corrective taxes. (Note, however, that if healthcare cost increases continue to outpace general inflation, this first rebuttal loses some force.) Second, since smokers on average die younger than nonsmokers, they reduce the drain on the public purse for social security payments and have fewer years of eligibility for (costly) Medicare.36See Jane G. Gravell and Dennis Zimmerman, Cigarette Taxes to Fund Health Care Reform: An Economic Analysis (Washington, DC: Library of Congress, 1994); and Willard G. Manning et al., “The Taxes of Sin: Do Smokers and Drinkers Pay Their Way?” JAMA 261, no. 11 (1989): 1604–9.
Thus it is unsurprising that studies taking these considerations into account while computing the optimal tax to account for fiscal externalities alone generally find that current excise tax levels are too high compared to the net externalities.37It is also important to note that studies (such as those cited in note 35) were reaching such conclusions well before the recent rounds of increases in tobacco taxes. See figure 2. Even using an astronomically high figure for the health cost to society of smoking a single pack ($35), the optimal tax to correct for negative externalities would be only 40 cents per pack (compared to the actual excise tax, which averaged around $2.80 in 2018).38For the average tax rate, see figure 2; for the study, see Jonathan Gruber and Botond Köszegi, A Modern Economic View of Tobacco Taxation (Paris: International Union against Tuberculosis and Lung Disease, 2008). This estimate of the net negative externality does not include any harmful effects of secondhand smoke. The weight of the literature instead finds similarly small externalities, but some notable exceptions actually find social savings from smoking (although these tend to be in countries with higher public expenditures on health than the United States).39Sijbren Cnossen, “Tobacco Taxation in the European Union,” FinanzArchiv/Public Finance Analysis 62, no. 2 (2006): 305–22.
However, fiscal externalities are not the only costs imposed on society by smokers. The other negative externality created by smoking is the burden imposed on nonsmokers, primarily through secondhand smoke. Such burdens include the annoyance of being exposed to others’ smoke and any adverse health effects. Health-related externalities based on second-hand smoke gained prominence in arguments for taxation and tobacco control in the US in the 1990s, after the earlier studies concluding that tobacco taxes were too high. Given that “everyone knows” how harmful secondhand smoke is, many people would be surprised to learn how weak the scientific evidence used to justify the indoor smoke-free laws of the 1990s actually was.40See W. Kip Viscusi, “The New Cigarette Paternalism,” Regulation 25, no. 4 (2002): 58–64; and Gary L. Huber, Robert E. Brockie, and Vijay K. Majhajan, “Smoke and Mirrors: The EPA’s Flawed Study of Environmental Tobacco Smoke and Lung Cancer,” Regulation 16, no. 3 (1993): 44–54. A landmark study in 1993 from the Environmental Protection Agency purported to show the adverse health effects of secondhand smoke and was influential in the passage of many local and state smoke-free ordinances. However, the report was savaged by a federal court.41A US district court found that the “EPA’s study selection is disturbing” and that the agency had cherry-picked the data, excluding almost half the available evidence—the half that did not support its preferred conclusion. See Flue-Cured Tobacco Co-op. v. U.S.E.P.A., 4 F. Supp. 2d 435 (M.D.N.C. 1998). While this court decision was later overturned for the reason that the EPA’s study was not a reviewable action under the Administrative Procedure Act, the findings regarding the scientific weakness of the report were left unrebutted. See Flue-Cured Tobacco Cooperative Stabilization Co. et al. v. Environmental Protection Agency et al., 313 F.3d 852 (4th Cir. 2002). The study, which stated that it reviewed the best available scientific evidence at the time, was thrown out by the court in part because it “did not demonstrate a statistically significant association between [secondhand tobacco smoke] and lung cancer,” which was its main claim. The point of rehearsing the story behind the first smoke-free ordinances is not to suggest that secondhand smoke does not have adverse health effects; that link is better established today. Rather, it is to note that, as is likely the case with the debate about e-cigarettes today (as will be covered below), the call to regulate smoking was sustained by political and social factors beyond those supported directly by the scientific knowledge at the time.42For a fascinating sociological perspective on why the anti-smoking crusade began to succeed when it did after “centuries of failure,” see Randall Collins, “Tobacco Ritual and Anti-ritual: Substance Ingestion as a History of Social Boundaries,” in Interaction Ritual Chains (Princeton, NJ: Princeton University Press, 2004). Collins points out the importance of nonscientific factors such as the “enjoying the moral prestige of a popular progressive movement” [p. 344].
Today, it is estimated that there are about 41,000 deaths per year in the United States attributable to secondhand smoke.43See The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General (Atlanta: US Department of Health and Human Services, 2014). Note that such estimates are typically reported without confidence intervals, but—given the uncertainty in the relative risks underlying the calculations—the confidence intervals would be wide. That figure represents about 1.5 percent of all deaths.44See Melanie Heron, “Deaths: Leading Causes for 2014,” National Vital Statistics Reports 65, no. 5 (2016): 1–95. The negative effects of maternal and passive smoking on infant and child health are considered some of the most important negative externalities.45See G. Banderali et al., “Short and Long Term Health Effects of Parental Tobacco Smoking during Pregnancy and Lactation: A Descriptive Review,” Journal of Translational Medicine 13 (2015); Kerry Anne McGeary et al., “Impact of Comprehensive Smoking Bans on the Health of Infants and Children,” American Journal of Health Economics 6, no. 1 (2020): 1–38. Various studies have associated smoking during pregnancy with reduced fetal growth, low birth weight, and, later in life, obesity, cardiovascular disease, and respiratory ailments. However, it remains the case that some of the links are weaker than people often assume. For example, one meta-analysis covering 76 studies on environmental tobacco smoke exposure found that there was no statistically significant association between environmental tobacco smoke in the home and premature births, low birthweight, spontaneous abortions, or lower Apgar scores at birth.46See Giselle Salmasi et al., “Environmental Tobacco Smoke Exposure and Perinatal Outcomes: A Systematic Review and Meta‐analyses,” Acta Obstetricia et Gynecologica Scandinavica 89, no. 4 (2010): 423–41. Note that the results regarding low birthweight are equivocal: while there is no statistically significant association between environmental tobacco exposure and low birthweight, when the latter is defined as a binary variable for birthweight less than 2.5 kilograms, there is a statistically significant association with lower birthweight when defined as a continuous variable. Such equivocal results hint at (perhaps substantial) nonlinearity or threshold effects in the relationship between environmental tobacco exposure and birthweight. Regardless, comparison with the results of other studies shows that the negative impact on birthweight of drinking one additional cup of coffee a day is more certain than the impact of a father smoking preterm (where certainty is ascertained by statistical significance and the width of confidence intervals). For the impact of a father smoking, see Ting-Jung Ko et al., “Parental Smoking during Pregnancy and Its Association with Low Birth Weight, Small for Gestational Age, and Preterm Birth Offspring: A Birth Cohort Study,” Pediatrics and Neonatology 55, no.1 (2014): 20–27. For the impact of drinking coffee, see Jongeun Rhee et al., “Maternal Caffeine Consumption during Pregnancy and Risk of Low Birth Weight: A Dose-Response Meta-analysis of Observational Studies,” PLOS ONE 10, no. 7 (2015): 1–18. On the other hand, the same meta-analysis found a positive association of secondhand smoke with congenital malformations.47The difficulty with measuring how detrimental maternal and passive smoking may be to neonatal and child health is exacerbated by the high likelihood that unobserved factors are correlated with these causes and the health outcomes. Most of the public health studies in the meta-analysis cited use cross-sectional data and cannot control for such confounding factors. A better-designed study demonstrates that the impact of maternal smoking on infant health and the infant healthcare cost savings associated with ceasing smoking during pregnancy are typically overestimated by an order of magnitude. See Douglas Almond, Kenneth Y. Chay, and David S. Lee, “The Costs of Low Birth Weight” Quarterly Journal of Economics 120, no. 3 (2005): 1031–83. Furthermore, many studies find that anti-smoking regulations are associated with better infant and child health.48See, for example, the many studies cited in Timor Faber et al., “Effect of Tobacco Control Policies on Perinatal and Child Health: A Systematic Review and Meta-Analysis” The Lancet Public Health 2, no. 9 (2017): e420–37 and Timor Faber et al., “Smoke-Free Legislation and Child Health” npj Primary Care Respiratory Medicine 26, art. no. 16067 (2016): 1–8. As discussed in the previous note, most such studies suffer potential bias from confounding factors. One recent study using methodology to reduce the impact of omitted variable bias (and, interestingly, one cited by a referee as bolstering the link between smoking and the health of infants and children) showed that after controlling for unobserved confounding factors at the county level, there was no association (at the standard 5% significance level) between comprehensive smoking bans and birthweight or the prevalence of low birthweight (see the bottom of panel b of table 3 of McGeary et al., “Impact of Comprehensive Smoking Bans.”) or the prevalence of hay fever, any respiratory allergies, asthma, ear infections, or being in “excellent or very good” general health. Out of nine child health outcomes studied, the only two displaying significant association with a ban were emergency room visits and being in “fair or poor” general health.
Before leaving the subject of negative externalities, it is important to note that a tax is a blunt instrument for reducing environmental tobacco smoke exposure. The price elasticity of market demand for cigarettes is estimated to be around 0.4, implying that a 10 percent increase in the price of cigarettes reduces total consumption in the market by only 4 percent. Other, more direct interventions can have much larger impacts. For example, consider concerns about the health of unborn children in a smoking household. One behavioral intervention that involved advising about health risks, introducing strategies within the home to eliminate exposure to smoke, and cognitive behavioral therapy for depression or intimate partner violence when necessary reduced the odds of secondhand smoke exposure by one-half.49Ayman El-Mohandes et al., “An Intervention to Reduce Environmental Tobacco Smoke Exposure Improves Pregnancy Outcomes,” Pediatrics 125, no. 4 (2010): 721–28. From the viewpoint of political economy, it is important to recognize that policymakers may prefer tobacco taxes to behavioral intervention programs because the former raise revenue for the state while the latter require public expenditure.
The behavioral rationale for regulation: “internalities.”
Since taxes on tobacco may already be adequate or too high from the usual point of view of taxing to correct for externalities, tobacco control advocates in recent years have turned to justifications based on behavioral economics. The nontechnical version of these arguments proceeds along the following lines: “Youth are not rationally forward-thinking consumers, and most smokers begin smoking in their youth.” The former assertion, coupled with the latter empirical observation, and supplemented with survey evidence showing that most smokers say that they wish they had not started smoking,50For example, roughly 90% of US smokers agreed with the following statement: “If you had to do it over again, you would not have started smoking.” Geoffrey T. Fong et al., “The Near-Universal Experience of Regret among Smokers in Four Countries: Findings from the International Tobacco Control Policy Evaluation Survey,” Nicotine & Tobacco Research 6, no. 3 (2004): 341–51. have led many advocates to call for higher tobacco taxes despite the absence of the usual economic rationales.
Arguments against this rationale include the observation that (as discussed earlier) taxes are blunt instruments to prevent smoking, especially since many youth do not pay for their cigarettes and, in particular, for their first cigarettes.51More than 60% of child smokers in one study said that they were given their first cigarettes. See Janet G. Baugh et al., “Development Trends of First Cigarette Smoking Experience of Children: The Bogalusa Heart Study,” American Journal of Public Health 72, no. 10 (1982): 1161–64. The greatest weight of a cigarette tax falls on adults, not youth. Furthermore, sales of tobacco to youth are already illegal; if the “infinite tax” tacitly imposed by a ban does not prevent youth from starting to smoke, then why would a finite tax do so—especially since both forms of tax can be evaded, as discussed below? The evidence is inconclusive regarding the impact of cigarette prices on youth smoking. At least some studies find that higher prices lower the propensity of youth to smoke,52Hana Ross and Frank J. Chaloupka, “The Effect of Cigarette Prices on Youth Smoking,” Health Economics 12, no. 3 (2003): 217–30; Dean R. Lillard, Eamon Molloy, and Andrew Sfekas, “Smoking Initiation and the Iron Law of Demand,” Journal of Health Economics 32, no. 1 (2013): 114–27. although other research indicates that the actual primary driver affecting youth’s smoking behavior is anti-smoking sentiment or regulations in the state rather than prices per se.53Philip DeCicca et al., “Youth Smoking, Cigarette Prices, and Anti‐smoking Sentiment,” Health Economics 17, no. 6 (2007): 733–49; Jeffrey Wasserman et al., “The Effects of Excise Taxes and Regulations on Cigarette Smoking,” Journal of Health Economics 10, no. 1 (1991): 43–64.
Extending the behavioral economic rationale for tobacco taxes to adults requires a theory involving so-called internalities—irrational behavior due to limited self-control or foresight. Such theories, when applied to tobacco consumption, assume that there is a “behavioral wedge” between the price of the good and the value to the consumer of the last unit consumed.54In the theories discussed here, the value to the consumer of the last unit consumed is measured as the money-metric marginal utility from consumption. See Emmanuel Farhi and Xavier Gabaix, “Optimal Taxation with Behavioral Agents,” American Economic Review 110, no. 1 (2020): 298–336. Whereas a rational consumer (roughly speaking) spends money on a commodity to the point where it is just worth it, in terms of satisfaction gained for the price paid, the behavioral wedge implies that the individual “overconsumes” the good, even as evaluated by the person’s own (eventual) preferences. Such individuals will look back on past decisions and wish that they had not consumed so much of the good. This may happen, for example, if youth, when they first try smoking, underestimate the likelihood that they will get addicted and become lifelong smokers (with all the resulting pecuniary and health costs). The implication is that, theoretically, increasing the price of a good by increasing an excise tax may actually increase some people’s welfare. Thus, a tax may help “nudge” a consumer toward an outcome that is better for that person, in the estimation of that person. One study adopting this approach arrived at the conclusion that an “optimal” tax to correct for internalities might be as high as $15 per pack—far higher than any tax in the nation.55Gruber and Köszegi, Modern Economic View of Tobacco Taxation. Such conclusions regarding optimal taxes make the behavioral approach a convenient rationale for parties advocating for higher tobacco taxes.
The paternalistic rationale for regulation.
As is clear from the discussion of the behavioral rationale for tobacco regulation, many policy analysts and policymakers approach the subject of tobacco regulation with a heavy dose of paternalism. They view smokers as faulty decision makers who need to be saved from their own poor choices. Some authors are quite explicit about this. For example, in one behavioral economic study performed for a lung cancer group, the authors explain, “we will focus on failures of individual self-control which lead to excessive smoking relative to desired levels. In such a case, tobacco taxation can provide a corrective force to combat failures of self-control.”56Gruber and Köszegi, Modern Economic View of Tobacco Taxation, p. 2. In this approach, the power of the state to tax provides a corrective force to nudge (or shove) irrational, tricked, or self-deluded smokers toward cessation.
Paternalism is a comfortable position for many policymakers to adopt, since—given smoking’s negative correlation with income and education—relatively few of them smoke today. As Kip Viscusi, a University Distinguished Professor at Vanderbilt University, has pointed out, since policymakers have chosen not to smoke, it is therefore easy for them to assume that smokers are mistaken, irrational, or in need of policy nudges toward cessation.57Viscusi, “New Cigarette Paternalism.” Of course, the fact that a behavior is hard to quit does not necessarily prove that the choice to begin was irrational (as most coffee drinkers would attest).58For a discussion of assumptions under which a rational individual would choose to become addicted, see Gary S. Becker and Kevin M. Murphy, “A Theory of Rational Addiction,” Journal of Political Economy 96, no. 4 (1988): 675–700. Furthermore, assumed faulty choices based on mistaken perceptions of the health effects of smoking appear to be unlikely, since, if anything, the American public overestimates the risks of smoking today.59Viscusi shows that at a time when medical science indicated that the risk of lung cancer for an average smoker was 6%–13%, the public thought it was 47%. Similar overestimation of risk is also present for premature mortality and life-years lost. Viscusi, “New Cigarette Paternalism.” (The evidence about whether youth in particular hold correct perceptions of the risks involved in smoking is inconclusive, however.)60The evidence in one study shows that among 14-to-22-year-olds, 70% of smokers and 79% of nonsmokers overestimated the risks of lung cancer. The same researchers found that only 34% of smokers and 41% of nonsmokers overestimated the total mortality risk of smoking, which the researchers take to be around 50%. Daniel Romer and Patrick Jamieson, “Do Adolescents Appreciate the Risks of Smoking? Evidence from a National Survey,” Journal of Adolescent Health 29, no. 1 (2001): 12–21. However, at the time of that study, the public was being told by the surgeon general’s report on smoking and the National Cancer Institute that the mortality risk was 18 percent to 36 percent. See Viscusi, “New Cigarette Paternalism.” It appears unlikely that any average smoker or nonsmoker would be looking at the technical academic or clinical literature indicating higher risk. Thus, the large majority of both smokers and nonsmokers were overestimating the risks compared to what they were being told by the most prominent sources of information. One would expect that as the higher estimates of mortality risk diffused into the public-facing messaging in the tobacco control community, people’s perceptions of risk would rise in response, if the degree of overestimation were to remain similar. However, apparently no more recent studies on risk perception have been performed.
Evidence for intertemporal irrationality and time inconsistency in decision-making (by which economists mean that the future self will regret decisions made by the present self) comes mainly from lab experiments. These are typically performed on college students at elite universities—hardly a representative demographic. There is also a small empirical literature that claims to find time inconsistency in real-world economic decisions (other than decisions about smoking).61For example, one strand of literature finds time inconsistency in labor market and welfare program participation decisions. See Hanming Fang and Dan Silverman, “Time‐Inconsistency and Welfare Program Participation: Evidence from the NLSY,” International Economic Review 50, no. 4 (2009): 1043–77. Such apparent irrationality follows from individuals in the data not making the choices that the economic theorists think that they should after estimating impressively technical yet still restrictive models of consumers’ choices. It remains to be seen whether these findings will hold up when more realistic models of economic behavior based on less restrictive assumptions are investigated.
While the arguments for paternalistic action by the state thus assume that smokers “need help helping themselves,” arguments for less paternalism can be based on normative and positive grounds.62See Russell S. Sobel and Joshua C. Hall, “In Loco Parentis: A Paternalism Ranking of the States,” in For Your Own Good: Taxes, Paternalism, and Fiscal Discrimination in the Twenty-First Century, ed. Adam J. Hoffer and Todd Nesbit (Arlington, VA: Mercatus Center at George Mason University, 2018). Normative ideas include the idea that the proper role of government is to protect the liberty of the citizens regarding—among other concerns—economic decisions, and the idea that (absent compelling reasons to the contrary) individuals should be free to make choices without government interference. Conversely, even granting the premise of limited cognition and the desire to optimize the behavior of individuals who cannot do so themselves, bounded rationality can raise the costs of government decision-making relative to private decision-making.63The argument follows from the observations that consumers have stronger incentives to correct their behavior than do government decision makers and that consumers have stronger incentives to make good choices when choosing what to buy than when choosing how to vote. See Edward L. Glaeser, “Paternalism and Psychology,” Regulation 29, no. 2 (2006). Positive arguments against paternalistic tobacco taxes are based on the unintended consequences that such taxes can have. For example, evidence from the 1990s indicates that higher prices caused smokers to switch to cigarettes that were higher in tar and nicotine, and therefore more harmful and addictive.64See M. C. Farrelly et al., “The Effects of Higher Cigarette Prices on Tar and Nicotine Consumption in a Cohort of Adult Smokers,” Health Economics 13, no. 1 (2004): 49–58. Despite the oft-heard slogan that “there is no such thing as a safer cigarette,” the epidemiological evidence indicates that low-tar cigarettes reduce the risk of lung cancer and total mortality for smokers. See G. C. Kabat, “Fifty Years’ Experience of Reduced-Tar Cigarettes: What Do We Know about Their Health Effects?,” Inhalation Toxicology 15, no. 11 (2003): 1059–102. Other unintended consequences are covered in the next subsection.65For more complete critiques of paternalism and taxation, see Adam J. Hoffer and Todd Nesbit, eds., For Your Own Good: Taxes, Paternalism, and Fiscal Discrimination in the Twenty-First Century (Arlington, VA: Mercatus Center at George Mason University, 2018); Adam J. Hoffer, William F. Shughart II, and Michael D. Thomas, “Sin Taxes and Sindustry: Revenue, Paternalism, and Political Interest,” Independent Review 19, no. 1 (2014): 47–64.
Unintended consequences of taxes and regulations.
An effective approach to policy must focus less on what policymakers hope will happen and more on what is likely to happen. This takes us into the realm of unintended consequences.
A standard desideratum for taxation is equity, based on the ability-to-pay principle. This principle leads to the system of progressive income taxation in the United States, for example. Excise taxes on cigarettes are regressive, however: poorer individuals spend a greater share of their income on consumption, and therefore an excise tax takes a greater share of a poor person’s income than it does of a wealthy person’s income. Furthermore, cigarette smoking is more prevalent among lower-income groups in the United States. These facts compound to make tobacco taxes doubly regressive.66See Matthew C. Farrelly et al., “Response by Adults to Increases in Cigarette Prices by Sociodemographic Characteristics,” Southern Economic Journal 68, no. 1 (2001): 156–65; Don Fullerton and Diane L. Rogers, Who Bears the Lifetime Tax Burden? (Washington, DC: Brookings Institution Press, 1993); Andrew B. Lyon and Robert M. Schwab, “Consumption Taxes in a Life-Cycle Framework: Are Sin Taxes Regressive?,” Review of Economics and Statistics 77, no. 3 (1995): 389–406; and Dahlia K. Remler, “Poor Smokers, Poor Quitters, and Cigarette Tax Regressivity,” American Journal of Public Health 94, no. 2 (2004): 225–29. While tobacco taxes may constitute only a small part of the total financial burden facing most smokers, in some cases the tax burden could be onerous. Consider, as an extreme example, a full-time minimum-wage worker in Chicago, where combined federal, state, county, and local tobacco taxes during the second half of 2019 were $8.17 per pack.67See “Increases and Changes to Consumer Taxes in Chicago for 2020,” Civic Federation, January 10, 2020, https://www.civicfed.org/civic-federation/blog/increases-and-changes-consumer-taxes-chicago-2020. The minimum wage in Chicago at the time was $12 per hour. During that period, the taxes alone on a pack-a-day smoking habit would have taken up 12 percent of the individual’s gross wages.68See Matthew C. Farrelly, James M. Nonnemaker, and Kimberly A. Watson, “The Consequences of High Cigarette Excise Taxes for Low-Income Smokers,” PLOS ONE 7, no. 9 (2012): e43838. The authors conclude after an empirical examination that high cigarette taxes “can impose a significant financial burden on low-income smokers.” See also James E. Prieger et al., The Impact of Ecigarette Regulation on the Illicit Trade in Tobacco Products in the European Union (Geneva, Switzerland: BOTEC Analysis, 2019), which discusses at length the issue of “specific impoverishment” caused by tobacco taxes.
If higher taxes encouraged many low-income individuals to quit smoking, then one could argue that the regressive impact of tobacco taxes would be blunted or removed entirely. The evidence for the predicate is weak, however. There is evidence that higher prices are associated with a lower number of smokers, even among the low-income population, but evidence for a link between prices and cessation is less clear (in part because cessation is harder to study than smoking prevalence). One study found that there is no correlation between successful cessation among smokers below the poverty line and cigarette prices in their state of residence, either in bivariate analysis or after controlling for other factors.69 Maya Vijayaraghavan et al., “The Effectiveness of Cigarette Price and Smoke-Free Homes on Low-Income Smokers in the United States,” American Journal of Public Health 103, no. 12 (2013): 2276–83. Furthermore, while some evidence shows that higher prices are associated with lower smoking prevalence among low-income individuals, this evidence does not by itself imply that taxes cause cessation, since it could just as well mean that fewer low-income individuals ever started smoking.
The indirect evidence for higher taxes leading to cessation is stronger: several studies show that tax increases lead to a lower smoking prevalence among older adults.71Philip DeCicca and Logan McLeod, “Cigarette Taxes and Older Adult Smoking: Evidence from Recent Large Tax Increases,” Journal of Health Economics 27, no. 4 (2008): 918–29. Given that few people begin smoking once out of their twenties, a lower prevalence of smoking among older smokers than younger smokers is indicative of cessation.72Even here, the evidence is mixed, because when the estimated smoking responses to tax increases are used to simulate trends in the prevalence of smoking in the US, the models greatly underpredict actual smoking rates. Philip DeCicca et al., “The Economics of Smoking Prevention,” in Oxford Research Encyclopedia of Economics and Finance (Oxford: Oxford University Press, 2018). That is, if tax increases discouraged adult smoking so much, then there would not be so many actual smokers still. Thus, DeCicca et al. conclude that “the true [price] elasticity lies between zero and −0.1, which is considerably smaller than the corresponding consensus estimate.” Regardless, another study found that, cigarette tax increases remain regressive even accounting for the different sensitivity among income groups of smoking to prices.73Gregory J. Colman and Dahlia K. Remler, “Vertical Equity Consequences of Very High Cigarette Tax Increases: If the Poor Are the Ones Smoking, How Could Cigarette Tax Increases Be Progressive?,” Journal of Policy Analysis and Management 27, no. 2 (2008): 376–400. This study also explains how under extreme behavioral models (as discussed earlier) cigarette taxes can be progressive, but nevertheless concludes that “taxes and other hindrances on smoking benefit higher-income more than lower-income smokers who are planning to quit.” Colman and Remler, “Vertical Equity Consequences,” 396.
Proponents of higher tobacco taxes often respond to the regressivity argument by contending that revenue from the taxes should be directed toward cessation programs intended to help low-income smokers quit or toward relieving these smokers’ financial burdens.74See, for example, Vijayaraghavan et al., “Effectiveness of Cigarette Price and Smoke-Free Homes.” Funding cessation programs may be an admirable intention, but—as mentioned earlier—less than 3 percent of current tobacco tax and MSA payments are spent on cessation.75See “State-by-State Look,” Campaign for Tobacco-Free Kids. While this fact may appear to be at odds with the common recent practice of earmarking tax increases for cessation programs or other public health initiatives, the fungibility of state tax revenue implies that earmarking a dollar does not mean that an additional dollar will be spent on the targeted cause. See George R. Crowley and Adam J. Hoffer, “Earmarking Tax Revenues: Leviathan’s Secret Weapon?,” in Hoffer and Nesbit, For Your Own Good. Taxing to relieve a household’s financial burden is an odd argument, since no scheme taxing a subset of the poor could result in net financial gains for those taxed. A final open question regarding the equity of taxes is whether the health benefits of reduced smoking accrue disproportionately to lower-income individuals and families. If so, the direct regressivity of the taxes would be attenuated (or even reversed) by the offsetting health benefits.
Illicit trade in response to tobacco taxes is also a concern. As stated in a leading economics textbook on public finance, “markets do not take taxes lying down.”76See Jonathan Gruber, Public Finance and Public Policy (New York: Worth Publishers, 2005), 547. Furthermore, to borrow a statement attributed to John Maynard Keynes, “the avoidance of taxes is the only pursuit that still carries any reward.” A large body of research indicates that increasing tobacco taxes can have the unintended consequence of stimulating illicit trade in tobacco products (ITTP).77See Roger Bate, Cody Kallen, and Aparna Mathur, “The Perverse Effect of Sin Taxes: The Rise of Illicit White Cigarettes,” Applied Economics 52, no. 8 (2020): 789–805; James E. Prieger and Jonathan Kulick, “Cigarette Taxes and Illicit Trade in Europe,” Economic Inquiry 56, no. 3 (2018): 1706–23; James E. Prieger and Jonathan Kulick, “Tax Evasion and Illicit Cigarettes in California: Part IV—Smokers’ Behavioral and Market Responses to a Tax Increase,” BOTEC Analysis, January 24, 2019, https://ssrn.com/abstract=3322095; Philip DeCicca, Donald Kenkel, and Feng Liu, “Excise Tax Avoidance: The Case of State Cigarette Taxes,” Journal of Health Economics 32, no. 6 (2013): 1130–41; Michael LaFaive, “Prohibition by Price: Cigarette Taxes and Unintended Consequences,” in Hoffer and Nesbit, For Your Own Good; and the numerous empirical studies cited in these studies. In the United States, most ITTP takes the form of legitimately manufactured cigarettes that are transported between states to be sold illicitly, avoiding state and local excise taxes at the point of retail sale. ITTP also involves counterfeit cigarettes, untaxed sales from Native American reservations, illicit whites (cigarettes legal in the country of manufacture but intended for illegal sales in other markets), and gray market reimported goods.78See James E. Prieger, Jonathan Kulick, and Mark A. R. Kleiman, “Unintended Consequences of Cigarette Prohibition, Regulation, and Taxation,” International Journal of Law, Crime and Justice 46 (2016): 69–85. ITTP is big business. The National Academy of Sciences found in 2017 that illicit sales compose between 8.5 percent and 21 percent of the total market for cigarettes in the United States. This range represents between 1.24 and 2.91 “billion packs of cigarettes annually and between $2.95 billion and $6.92 billion in lost gross state and local tax revenues.”79National Research Council and Institute of Medicine, Understanding the U.S. Illicit Tobacco Market: Characteristics, Policy Context, and Lessons from International Experiences, ed. Peter Reuter and Malay Majmundar (Washington, DC: National Academies Press, 2015), 4. Worldwide, the avoided taxes from ITTP are estimated to be in the tens of billions of dollars per year, putting ITTP in the same financial class as the global traffic in illicit drugs.80See discussion of this comparison in Prieger et al., Impact of Ecigarette Regulation.
The economic explanation for ITTP is simple: licit and illicit cigarettes are substitutes, and when the tax-inclusive price of the licit good rises, some users will switch to the illicit substitute. The degree to which tax increases and tax differentials among states and localities cause substitution toward ITTP depends on many factors, including the rule of law, enforcement at customs borders and at points of sale, the ease of access to illicit sources, the price differential between licit and illicit cigarettes, and the moral sentiments of the smoker.81For empirical evidence on the final point, see Prieger and Kulick, “Tax Evasion and Illicit Cigarettes in California: Part IV.”
While the basic fact that an increase in taxes leads to more ITTP, holding other factors constant, is generally accepted by most economists, there is much disagreement over the policy implications. If tax rates across states were unified, then presumably raising a unified rate would not stimulate as much ITTP as raising an already high local tax (such as in Chicago or New York City), given the large role that interstate tax arbitrage currently plays in ITTP.82Rajiv Goel and James W. Saunoris, “Cigarette Smuggling: Using the Shadow Economy or Creating Its Own?,” Journal of Economics and Finance 43 (2019): 582–93. Some in the public health community downplay any suggestion that taxes are linked to ITTP, dismissing the argument through guilt by association, since the tobacco industry makes this claim.83See Julia Smith, Sheryl Thompson, and Kelley Lee, “Death and Taxes: The Framing of the Causes and Policy Responses to the Illicit Tobacco Trade in Canadian Newspapers,” Cogent Social Sciences 3, no. 1 (2017). Others argue either that the effects are small or that other measures can be taken to combat illicit trade.84See Luk Joossens and Martin Raw, “From Cigarette Smuggling to Illicit Tobacco Trade,” Tobacco Control 21, no. 2 (2012): 230–34. Careful empirical investigation has shown, however, that raising taxes can lead to sizeable increases in ITTP.85See in particular Prieger and Kulick, “Cigarette Taxes and Illicit Trade in Europe.” Notwithstanding, the evidence is clear that in most cases ITTP may erode but does not reverse revenue gains from increased taxes. Similarly, taxes do decrease consumption of tobacco products, even though ITTP may attenuate the amount by which they do so.86A group of economists with diverse perspectives on tobacco taxation and ITTP state that “little disagreement exists that an increase in the tax rate would generate significant increases in revenue, or that it would decrease consumption.” Warner et al., “Criteria for Determining an Optimal Cigarette Tax.”
Before leaving the subject of ITTP, it is important to note that it creates harms to health additional to those of smoking genuine, fully taxed cigarettes. Counterfeit cigarettes have been shown to contain pesticides, human and animal waste, heavy metals, and other harmful substances.87See Lee Moran, “Fake Cigarettes Containing Human Feces, Rat Droppings Flood British Market: Report,” New York Daily News, November 11, 2014; W. Edryd Stephens, Angus Calder, and Jason Newton, “Source and Health Implications of High Toxic Metal Concentrations in Illicit Tobacco Products,” Environmental Science and Technology 39, no. 2 (2005): 479–88; and Oliver Bennett, “How Counterfeit Cigarettes Containing Pesticides and Arsenic Make It to Our Streets,” Independent, August 7, 2018. Furthermore, law enforcement directed at ITTP can create other harms, including those from incarceration and violence, given the well-known link between enforcement action against illicit drug markets and violence.88See Prieger, Kulick, and Kleiman, “Unintended Consequences of Cigarette Prohibition”; James E. Prieger and Jonathan Kulick, “Violence in Illicit Markets: Unintended Consequences and the Search for Paradoxical Effects of Enforcement,” B.E. Journal of Economic Analysis and Policy 15, no. 3 (2015): 1263–95; and James Prieger and Jonathan Kulick, “Unintended Consequences of Enforcement in Illicit Markets,” Economics Letters 125, no. 2 (2014): 295–97.
Issues Involved with Taxing and Regulating E-cigarettes
This section reviews the most prominent issues regarding the regulation of ENDS and potential unintended consequences.
The main issues surrounding vaping concern its safety, its relationship to smoking (including whether it is a promising avenue for harm reduction), and unintended consequences of regulation and taxation. Harm reduction refers to policies and approaches aimed at reducing the harms from an addictive substance, but not the use of the substance per se.89See Alison Ritter and Jacqui Cameron, “A Review of the Efficacy and Effectiveness of Harm Reduction Strategies for Alcohol, Tobacco and Illicit Drugs,” Drug and Alcohol Review 25, no. 6 (2006): 611–24. The viewpoint of harm reduction is widely accepted in the public health community for alcohol and illicit drugs, but it is controversial in the tobacco control community, mainly because of guilt by association with Big Tobacco, which “has been seen by some to lead the harm reduction push (through the development of new nicotine delivery devices).”90Ritter and Cameron, “Review of the Efficacy and Effectiveness,” 613. Thus, in traditional tobacco control abstinence is taken as the goal, rather than finding safer ways to consume nicotine. The rejection of harm reduction as a guiding philosophy is sometimes justified with reference to the precautionary principle, which posits that lack of scientific certainty should not delay action to regulate or ban new products such as e-cigarettes.91See the discussion of harm reduction versus the precautionary principle in Lawrence W. Green, Jonathan E. Fielding, and Ross C. Brownson, “The Debate about Electronic Cigarettes: Harm Minimization or the Precautionary Principle,” Annual Review of Public Health 39 (2018): 189–91. Notwithstanding, the discussion to follow examines the issue through the lens of harm reduction and whether e-cigarettes could be part of such an approach.
Is vaping safer than smoking?
What many consider to be the most important question is the easiest to answer: Is vaping safer than smoking? Because e-cigarettes do not involve combustion, and because the combustion of the organic material in a cigarette creates nearly all the health hazards, it would be surprising indeed if e-cigarettes were found to be as risky for health as smoking. This simple expectation has been greatly muddied in the public mind by certain public health advocates who hold a priori goals of abstinence for both smoking and vaping. Thus, a review of the state of current knowledge on this topic may be useful.
To begin with, from the standpoint of harm reduction, the question is not whether e-cigarettes pose no health risks at all (except perhaps for the subject of initiation by youth, a subject to which I will return below). In the context of the public health disaster caused by smoking, the proper first question must be whether e-cigarettes are safer than cigarettes, and to what degree. After considering the state of the evidence, the official health ministry of England declared that vaping is at least 95 percent less harmful to health than smoking.92See A. McNeill et al., Ecigarettes: An Evidence Update (London: Public Health England, 2015). The purpose of Public Health England’s statement in 2015 was not to present a precise risk multiple, but instead to effectively encourage smokers who have been unable to quit by other methods to switch to vaping instead of smoking.93“Based on current knowledge, stating that vaping is at least 95% less harmful than smoking remains a good way to communicate the large difference in relative risk unambiguously so that more smokers are encouraged to make the switch from smoking to vaping.” McNeill et al., Ecigarettes: An Evidence Update. Given the clarity of the statement, the obvious implication that switching should be encouraged, and the resistance of some in the American public health community to that message, it is unsurprising that Public Health England has been attacked for its statement. See, for example, Thomas Eissenberg et al., “Invalidity of an Oft-Cited Estimate of the Relative Harms of Electronic Cigarettes,” American Journal of Public Health 110, no. 2 (2020): 161–62. A good discussion of the issues involved and a rebuttal may be found in Clive Bates, “Vaping Is Still at Least 95% Lower Risk than Smoking—Debunking a Feeble and Empty Critique,” The Counterfactual (blog), January 17, 2020.
Eliquids and vapor contain substances known to be harmful to human health when inhaled, including irritants, carcinogens, and particulates.94Tianrong Cheng, “Chemical Evaluation of Electronic Cigarettes,” Tobacco Control 23, no. S2 (2014): 11–17. Then again, much of modern life exposes individuals to harmful substances. Thus the question is what the short- and long-term health effects from such exposure are, and how they compare with those from smoking.
One difficulty in discussing the health effects of vaping is the great multiplicity of products: there is no “standard” vapor, concentration of chemicals in eliquids, or intensity of inhalation. Notwithstanding, one study found that along the spectrum of products tested, the preponderance of products produced vapor with cancer potencies of less than 1 percent of those of tobacco smoke.95William E. Stephens, “Comparing the Cancer Potencies of Emissions from Vapourised Nicotine Products Including Ecigarettes with Those of Tobacco Smoke,” Tobacco Control 27, no. 1 (2018): 10–17. Fewer harmful substances in the vapor means that fewer end up in the body. Another study concluded that switching completely from cigarettes to e-cigarettes “substantially reduced levels of measured carcinogens and toxins” in the body.96See Lion Shahab et al., “Nicotine, Carcinogen, and Toxin Exposure in Long-Term Ecigarette and Nicotine Replacement Therapy Users: A Cross-Sectional Study,” Annals of Internal Medicine 166, no. 6 (2017): 390–400. Overall, the National Academy of Sciences report on e-cigarettes found that “there is conclusive evidence that completely substituting e-cigarettes for combustible tobacco cigarettes reduces users’ exposure to numerous toxicants and carcinogens present in combustible tobacco cigarettes.”97See National Academies of Science, Engineering, and Medicine, Public Health Consequences of Ecigarettes.
Perhaps the strongest case against vaping on the grounds of deleterious health effects would be based on respiratory disease, since exposure to particulates and flavorings in e-cigarette vapor could potentially impair the function of the lungs. Several studies find that vaping can cause acute respiratory symptoms such as coughing and wheezing, particularly among adolescents. Some of these studies do not control for concurrent or past smoking; controlling for these confounding factors removes the positive associations between vaping and respiratory symptoms in some studies.98For example, one study found that the odds of wheezing in adolescents are affected by ecigarette use only when past cigarette use is not controlled for. See Rob McConnell et al., “Electronic Cigarette Use and Respiratory Symptoms in Adolescents,” American Journal of Respiratory and Critical Care Medicine 195, no. 8 (2017): 1043–49. Conversely, the association between vaping and the odds of having symptoms of bronchitis was reduced in magnitude but not removed when past cigarette use was controlled for. Even here, however, the recent National Academy of Sciences report concluded that “there is no available evidence whether or not e-cigarettes cause respiratory diseases in humans.”99See National Academies of Science, Engineering, and Medicine, Public Health Consequences of Ecigarettes. Conversely, the same report found “limited evidence” for improvement in symptoms from asthma and chronic obstructive pulmonary disease when smokers who suffered from those ailments switched completely to vaping. Summarizing evidence concerning a variety of potential ill health effects, the report found that there is “substantial evidence that completely switching from regular use of combustible tobacco cigarettes to e-cigarettes results in reduced short-term adverse health outcomes in several organ systems,” including the respiratory system.
To conclude, while there is great uncertainty about the long-term effects of vaping, the answer to whether using e-cigarettes is better for health than smoking is almost surely yes. Viewed as part of a continuum of nicotine delivery methods arranged in terms of health risk, e-cigarettes appear to be much closer to nicotine replacement therapies than to smoking. However, the strongest arguments for the potential for e-cigarettes to reduce health harms to users can be made for users who switch completely away from smoking. There is no available evidence about whether long-term e-cigarette use among users who continue to smoke, called dual users, changes morbidity or mortality compared to smokers who do not vape.100See National Academies of Science, Engineering, and Medicine, Public Health Consequences of Ecigarettes.
Do e-cigarettes aid in cessation?
Is vaping a useful aid to help smokers quit smoking, or does it just prolong the habit by allowing smokers another way to consume nicotine when they are temporarily unable to smoke? It appears likely that e-cigarettes would be a more appealing cessation aid than nicotine replacement therapies (NRTs) such as patches, gum, or lozenges, given the sensory and behavioral similarity of vaping to smoking. The scientific literature on e-cigarettes and cessation is still in its early stages; given the novelty of vaping, no long-term studies on e-cigarettes and cessation have been performed. However, the initial literature is mainly encouraging.
A review of existing studies conducted in 2015 found that, overall, use of e-cigarettes was positively associated with both cessation of smoking and reduction in the intensity of smoking (for those who did not quit).101See Muhammad Aziz Rahman et al., “Ecigarettes and Smoking Cessation: Evidence from a Systematic Review and Meta-analysis,” PLOS ONE 10, no. 3 (2015). A more recent review of studies on cessation came to a similar conclusion, but only after excluding numerous published studies that did not meet standard levels of quality for scientific research in medicine or public health.102See Andrea C. Villanti et al., “How Do We Determine the Impact of E‐cigarettes on Cigarette Smoking Cessation or Reduction? Review and Recommendations for Answering the Research Question with Scientific Rigor,” Addiction 113, no. 3 (2018): 391–404. The observation that this review found that most studies on vaping and cessation (all but four out of 91) failed to constitute reliable scientific evidence is important, because public health researchers who oppose vaping sometimes claim that “the weight of the evidence” shows that ecigarette use does not aid cessation. The latter meta-analysis found that rates of smoking cessation with e-cigarettes were generally similar to rates of cessation with NRT, while the former found e-cigarettes to be twice as effective as NRT.103The cessation rate, defined as the 12-month quit rate, was found to be about 10% with NRTs and 20% with ecigarettes. See Rahman et al., “Ecigarettes and Smoking Cessation.” Some research conducted after these reviews also suggests that e-cigarettes can play a role in cessation.104Some recent studies finding that ecigarettes may aid cessation use quasi-experimental designs. See Dhaval Dave et al., “Does Ecigarette Advertising Encourage Adult Smokers to Quit?,” Journal of Health Economics 68 (2019): 102227; Henry Saffer et al., “Ecigarettes and Adult Smoking: Evidence from Minnesota” (NBER Working Paper No. 26589, National Bureau of Economic Research, Cambridge, MA, December 2019). Other studies employ randomized controlled trials. See Peter Hajek et al., “A Randomized Trial of Ecigarettes versus Nicotine-Replacement Therapy,” New England Journal of Medicine 380 (2019): 629–37. The authors find that ecigarettes were more effective for smoking cessation than nicotine-replacement therapy.
Are kids getting addicted to e-cigarettes?
There have been many dire, headline-grabbing reports issued in recent years referring to the “vaping epidemic” among youth. For example, in 2019 many variations on the headline “Teen Vaping Surges to More Than One in Four Students” appeared.105See, for example, Angelica LaVito, “CDC Says Teen Vaping Surges to More than 1 in 4 High School Students,” CNBC, September 12, 2019. However, the much-publicized “27 percent” statistic pertains to the proportion of high school students who have used an e-cigarette once or more during the past 30 days. There is clearly a lot of casual use among high schoolers, since the prevalence of substantial use of e-cigarettes among high school students (defined as use on 20 or more days out of the past 30) is less than 10 percent.106Karen A. Cullen et al., “Ecigarette Use among Youth in the United States, 2019,” JAMA 322, no. 21 (2019): 2095–103. This figure is derived by multiplying the any-use prevalence of 27.5% by the proportion of current users using 20 days or more out of the past 30 (34.2%).
Furthermore, substantial use of e-cigarettes is mostly confined to youth who already smoke. Among students who had never tried any actual tobacco product in 2018, the prevalence of substantial use of e-cigarettes was found to be only 1.0 percent.107Robert West, Jamie Brown, and Martin Jarvis, “Epidemic of Youth Nicotine Addiction? What Does the National Youth Tobacco Survey Reveal about High School Ecigarette Use in the USA?,” Qeios preprint, submitted October 7, 2019. For such never-smokers, only 3.8 percent reported craving nicotine and only 3.1 percent reported wanting to use an e-cigarette within 30 minutes of waking. Combined with evidence that most dual-using high schoolers began with smoking, not vaping (see the next subsection), the researchers computing these statistics conclude that the data “do not support claims of a new epidemic of nicotine addiction stemming from use of e-cigarettes.”108West, Brown, and Jarvis, “Epidemic of Youth Nicotine Addiction?” Nevertheless, the prevalence of vaping—however it is measured—continues to rise among youth, and consequently it will require continued monitoring.
Finally, it is worth noting that not all youth vaping represents net health harms to the individual and society, given that in a counterfactual “no e-cigarettes” world, some young vapers would be smokers instead (or, in the case of dual use, potentially heavier smokers). The relationship between vaping and smoking is discussed in the next subsection.
Does vaping lead to smoking among youth?
The findings discussed in the previous subsection that most e-cigarette use by youth is by smokers, coupled with other evidence that the same is true for adults,109See, for example, Scott R. Weaver et al., “Use of Electronic Nicotine Delivery Systems and Other Tobacco Products among USA Adults, 2014: Results from a National Survey,” International Journal of Public Health 61, no. 2 (2016): 177–88. lead to the question of which came first. Does vaping lead to smoking (the “gateway hypothesis”), or do underage smokers just find vaping a more convenient (and likely cheaper)110Given that cigarette taxes are generally higher than taxes on ecigarettes (if there are any), among other reasons, vaping is generally seen as cheaper than smoking. Depending on the cigarettes and vaping device or method compared, the cost differences can be very large. See, for example, Ethan Wolff-Mann, “Vaping Is 95% Healthier and 40% Cheaper Than Smoking,” Money, August 20, 2015; and Lindsay Fox, “Smoking vs. Vaping: The Ultimate Cost Comparison,” EcigaretteReviewed (blog), February 25, 2016. way to consume nicotine while at school or elsewhere? First, it should be noted that many of the claims that e-cigarette use “causes” smoking are based on nothing more than the observation in population studies that many youth are dual users. However, it is likely that part of the association between vaping and smoking among youth is due to smoking leading to vaping. Another large part of the association is likely due to underlying (confounding) factors (such as a desire for risk-taking or exposure to smoking family members or peers) that make a youth more likely to vape and smoke.111This is known as the common liability hypothesis. See Lynn T. Kozlowski and Kenneth E. Warner, “Adolescents and Ecigarettes: Objects of Concern May Appear Larger Than They Are,” Drug and Alcohol Dependence 174 (2017): 209–14.
Given that it is unethical to perform randomized controlled trials involving exposure to vaping on youth, evidence can only come from observational studies of the population. Such studies, however, are inescapably beset by potential confounding factors. Population studies can control for certain observable demographic and behavioral confounders. Studies doing so that follow youth over time who do not initially smoke find that there is, in the estimation of the National Academy of Sciences report, “substantial evidence” that e-cigarette use increases the risk of trying cigarettes among youth and young adults.112National Academies of Science, Engineering, and Medicine, Public Health Consequences of Ecigarettes. However, it is impossible to control for all of the many genetic, behavioral, psychological, and environmental factors that surely must influence the propensities to smoke and vape, and none of the studies use econometric techniques designed to give some assurance that causal effects were identified. Some researchers, therefore, conclude that the association between vaping and smoking is more likely to be spurious than to be evidence for the gateway hypothesis.113See Jean-Francois Etter, “Gateway Effects and Electronic Cigarettes,” Addiction 113, no. 10 (2018): 1776–83. As better data and more sophisticated statistical techniques are brought to bear on this question, it may be hoped that researchers, policy-makers, and the public can place greater confidence on one conclusion or the other.
If the conclusion in the National Academy of Sciences report is statistically meaningful, one would expect that as vaping among youth has risen, so will have youth smoking rates. This is not the case, however. Simply put, youth smoking initiation has been falling while the prevalence of vaping has been rising. A recent trend analysis of the relationship between vaping and youth smoking found that “while trying electronic cigarettes may causally increase smoking among some youth, the aggregate effect at the population level appears to be negligible.”114See D. T. Levy et al., “Examining the Relationship of Vaping to Smoking Initiation among US Youth and Young Adults: A Reality Check,” Tobacco Control 28, no. 6 (2019): 629–35. Furthermore, the criterion of temporal precedence for causality states that if vaping causes smoking, then vaping must come before smoking. However, for the great majority of high school smokers, cigarettes were tried before e-cigarettes.115West, Brown, and Jarvis, “Epidemic of Youth Nicotine Addiction?” In 2014, only 2 percent of current high school age e-cigarette users who had smoked at least 25 cigarettes in their lifetimes said that they began with e-cigarettes. In 2015, that proportion had risen, but was still only between 8 percent and 15 percent.116West, Brown, and Jarvis, “Epidemic of Youth Nicotine Addiction?” The relevant survey question was not asked in more recent waves of the relevant survey.
Another way to pose the question is whether restrictions on youth access to e-cigarettes will decrease smoking. The scant evidence on this subject appears to point to the opposite conclusion. Imposing minimum age laws for sales of e-cigarettes is estimated to have increased youth smoking participation by about one percentage point, which suggests that some youth who otherwise would have purchased e-cigarettes either began smoking or failed to quit.117Similarly sized effects were found by two studies. See Dhaval Dave, Bo Feng, and Michael F. Pesko, “The Effects of E-cigarette Minimum Legal Sale Age Laws on Youth Substance Use,” Health Economics 28, no. 3 (2019): 419–36; A. S. Friedman, “How Does Electronic Cigarette Access Affect Adolescent Smoking?,” Journal of Health Economics 44 (2015): 300–308. Evidence in a similar vein comes from another study of underage rural girls: laws restricting sales of e-cigarettes to youth increased the prevalence of smoking during pregnancy by 0.6 percentage points, and evidence indicates that the cause was reduced cessation of smoking.118Michael F. Pesko and Janet M. Currie, “Ecigarette Minimum Legal Sale Age Laws and Traditional Cigarette Use among Rural Pregnant Teenagers,” Journal of Health Economics 66 (2019): 71–90. Given that the goal of minimum age laws is not just to discourage vaping but ultimately to improve health, these iatrogenic effects partially dilute the benefits of such laws.
Will the new federal minimum age law reduce youth vaping?
People between 18 and 21 years of age could legally purchase e-cigarettes in the majority of states at the beginning of 2019 (see figure 3), whereas none of them could a year later. How much the new age restrictions will reduce vaping among youth is as yet unknown. On the basis of previous experience with tobacco minimum age laws, we should expect that without enforcement the new law will have little to no effect on underage use.119Nancy A. Rigotti, “Youth Access to Tobacco,” Nicotine and Tobacco Research 1, suppl. 2 (1999): S93–S97. With enforcement, it is natural to expect that youth vaping would decline at least to some extent, if experience with earlier tobacco laws and youth smoking is any guide.120There is remarkably little evidence on this topic from the US context. Nancy Rigotti reports on two controlled studies from the US: In one, enforcement of minimum age laws to purchase tobacco had no effect on youth smoking, but in the other, enforcement was associated with lowering the growth rate of youth smoking. Rigotti, “Youth Access to Tobacco.” The 2015 National Academies study on the issue found no studies at all on the topic in the US but cited evidence from Europe that minimum age laws reduce youth smoking prevalence. Richard J. Bonnie, Kathleen Stratton, and Leslie Y. Kwan, eds., Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products (Washington, DC: National Academies Press, 2015).
However, several factors suggest that the minimum age laws will not eliminate use by underage vapers. First, most youth do not buy their own e-cigarettes at retail stores, since in most places those under 18 have already been disallowed from purchasing them since 2016; acquiring e-cigarettes from social sources (e.g., friends and family) is much more common.121Only 10.5% of 15-to-17-year-old vapers bought their own ecigarettes; it is much more common that they asked someone to buy on their behalf (17.3%) or got them from someone else (57%). Susanne Tanski et al., “Youth Access to Tobacco Products in the United States: Findings from Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health Study,” Nicotine and Tobacco Research 21, no. 12 (December 2019): 1695–99. See similar evidence from Hannah M. Baker et al., “Youth Source of Acquisition for Ecigarettes,” Preventive Medicine Reports 16 (2019); and Jessica K. Pepper et al., “How Do Adolescents Get Their Ecigarettes and Other Electronic Vaping Devices?,” American Journal of Health Promotion 33, no. 3 (2019). However, the hope of those raising the legal purchasing age is that younger teens will have fewer members of their social sourcing networks who are over 21. Furthermore, many youth who vape have already demonstrated willingness to break the law. Over two-fifths of youth who use e-cigarettes report vaping THC (tetrahydrocannabinol), which is illegal for youth even in states that have legalized cannabis.122Amy Fairchild et al., “Evidence, Alarm, and the Debate over Ecigarettes,” Science 366, no. 6471 (December 2019): 1318–20. Finally, even in relatively high-enforcement states such as California, approximately 7 percent of stores in 2018 were willing to sell e-cigarettes illegally to underage vapers.123Lisa Henriksen et al., “Assurances of Voluntary Compliance: A Regulatory Mechanism to Reduce Youth Access to Ecigarettes and Limit Retail Tobacco Marketing,” American Journal of Public Health 110, no. 2 (2020): 209–15. This latter finding is in accord with research showing that the majority (75%) of underage smokers who attempt to purchase tobacco in the US are not refused because of age.124Tanski et al., “Youth Access to Tobacco Products.”
Does vaping create externalities?
As discussed earlier, a classic argument for taxing tobacco rests on health harms created by secondhand smoke. What about secondhand exposure to vapor from e-cigarettes, or even thirdhand exposure to chemical residue that settles from vapor onto surfaces? If secondhand and thirdhand exposure create large health harms, then taxes on e-cigarettes and restrictions on where they can be used may be justified.
Given that the health harms of vaping are not yet known with precision, it is unsurprising that the secondary and tertiary health impacts are also largely unknown, at least in the sense that no “optimal tax” can be calculated yet to align private and social incentives. One systematic review of the scientific literature led to no stronger a statement than that second- and thirdhand exposure to vapor from e-cigarettes has “the potential to lead to adverse health effects.”125Isabel M. R. Hess, Kishen Lachireddy, and Adam Capon, “A Systematic Review of the Health Risks from Passive Exposure to Electronic Cigarette Vapour,” Public Health Research and Practice 26, no. 2 (2016). Emphasis added. The influential National Academy of Sciences report concluded that using an e-cigarette indoors “may involuntarily expose non-users to nicotine and particulates” but also that the effects of such exposure remain unknown.126National Academies of Science, Engineering, and Medicine, Public Health Consequences of Ecigarettes. Even if exposure to others’ vapor proves eventually to be harmful, it is highly likely to be less harmful than exposure to secondhand smoke. The two studies just cited state that the “risk from being passively exposed to . . . vapor is likely to be less than the risk from passive exposure to conventional cigarette smoke”127Hess, Lachireddy, and Capon, “Systematic Review of the Health Risks.” and that there is “moderate evidence that secondhand exposure to nicotine and particulates is lower from e-cigarettes compared with combustible tobacco cigarettes.”128National Academies of Science, Engineering, and Medicine, Public Health Consequences of Ecigarettes. Note also that the careful (and carefully worded) conclusions of these scientific assessments stand in contrast to statements by the World Health Organization, which comes down strongly against vaping. The World Health Organization answered the question “are secondhand ENDS emissions dangerous?” unequivocally: “Yes. The aerosols in ENDS typically contain toxic substances, including glycol which is used to make antifreeze. ENDS pose risks to users and non-users.” World Health Organization, “Q&A Detail: Ecigarettes,” accessed January 23, 2020, https://www.who.int/news-room/q-a-detail/e-cigarettes-how-risky-are-they. (The “yes” in the answer was later removed.) For discussion of the merits of this statement, see Clive Bates, “World Health Organisation Fails at Science and Fails at Propaganda—the Sad Case of WHO’s Anti-vaping Q&A,” The Counterfactual (blog), January 30, 2020.
Do restrictions on advertising tobacco apply to e-cigarettes? Should they?
Many of the restrictions on advertising tobacco do not apply to e-cigarettes, since the most important restrictions—most notably, the ban on advertising cigarettes on television and radio—are not FDA regulations. When the FDA deemed e-cigarettes to be tobacco products, any regulations promulgated by that agency thenceforth applied to e-cigarettes. Thus, since 2018, by federal law all advertisements for e-cigarettes must display the warning that “This product contains nicotine derived from tobacco. Nicotine is an addictive chemical.” The notice must occupy at least 20 percent of the area of the advertisement.129See Required Warning Statement Regarding Addictiveness of Nicotine, 21 C.F.R. 1143.3 (April 1, 2019). However, there is no federal law against advertising e-cigarettes on television, radio, websites, billboards, public transportation, and other outdoor venues, whereas these advertisements are prohibited in most of the US for cigarettes.130The television and radio ad ban for cigarettes is nationwide (under a federal law—it is not an agency regulation), but the other use of the venues mentioned is prohibited under the Tobacco Master Settlement Agreement, which applies in 46 states. Andrew Glass, “Congress Bans Airing Cigarette Ads, April 1, 1970,” Politico, April 1, 2018. Some states, however, ban advertising e-cigarettes on billboards.
Whether advertising e-cigarettes helps or hinders public health depends on how youth and adults respond to advertising, the health effects of vaping, and whether smokers use e-cigarettes to aid cessation. One recent study found that viewing television (but not magazine) advertising of e-cigarettes encouraged smokers to quit, with most of the effect due to greater success per quit attempt rather than to an increase in attempts.131See Dhaval Dave et al., “Does E-Cigarette Advertising Encourage Adult Smokers to Quit?” Journal of Health Economics 68 art. no. 102227 (2019):1–13. The authors estimate that 3 percent of the decrease in the prevalence of adult smoking is due to television advertising. This evidence, which the authors call “tentative” since it was gathered from a relatively short period (two years of data), should give policymakers pause if they are considering indiscriminate bans on advertising e-cigarettes. Whether and how ads targeting or particularly attractive to youth can be prevented without banning all advertising remains an open question, both for vaping and for other goods, such as alcohol.132See, for example, Michele Simon, “Reducing Youth Exposure to Alcohol Ads: Targeting Public Transit,” Journal of Urban Health 85, no. 4 (2008): 506–16.
What about the recent health scares involving vaping and lung illness?
In mid-2019, a spate of visits to emergency rooms around the country linked vaping to acute lung injuries, and the government responded promptly—by creating an acronym for the phenomenon: e-cigarette- or vaping-associated lung injury (EVALI). While by the end of the year the tide of cases of illness and death from EVALI appeared to be receding, the highly publicized events raised the issue of the health effects of e-cigarettes to prominence in the public’s eye. As I write this chapter, officials are still investigating the causes of EVALI, and given that products of questionable legality appear to be involved in many cases, the true causes may never be nailed down. However, the following paragraphs summarize what seems to be known at the present.
As of February 18, 2020, there were 2,739 hospitalizations and 68 deaths connected with EVALI.133The information here and the statistics to follow are from the Centers for Disease Control and Prevention’s information page, “Outbreak of Lung Injury Associated with the Use of Ecigarette, or Vaping, Products,” accessed October 9, 2020, https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. The Centers for Disease Control and Prevention is a part of the US Department of Health and Human Services. The emergency room visits rose sharply in August 2019 and peaked in September. Note that since e-cigarette usage had been growing smoothly and steadily since at least 2006, a suddenly appearing (and declining) epidemic such as EVALI cannot logically be caused by vaping in general. The most plausible current guess about the cause of EVALI centers on vitamin E acetate, a chemical added to e-cigarettes containing THC (loosely speaking, “marijuana vapes”) that the Centers for Disease Control and Prevention says is “strongly linked to the EVALI outbreak.” In government tests, 48 of 51 EVALI patients examined had vitamin E acetate in their lung fluid, compared to none found in a comparison group of 99 healthy people.134See Blount, et al., “Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI,” New England Journal of Medicine 382, no. 8 (2020):697-705. If the test group with EVALI were typical of the general population of vapers with regard to the presence of vitamin E acetate in their lungs, as would be the case if vitamin E acetate (and hence THC) had nothing to do with the illnesses, then the probability of observing no vitamin E acetate in the control group is a vanishingly small number: 1.5 × 10−122—a zero followed by a decimal point and 121 more zeroes. Of the roughly 2,000 EVALI patients for whom data were available, 82 percent reported using THC-containing products; given that such products are illegal in some places under state law and illegal everywhere under federal law, this percentage is undoubtedly lower than the actual proportion of THC vapers. Of those using THC-containing products, 84 percent reported acquiring products from informal sources other than physical commercial sources such as dispensaries and vape shops: friends, dealers, off the street, or online sellers.135The total percentage cited includes 6 percent who reported acquiring products from both commercial and informal sources. Furthermore, the most commonly used brand in a sample of 86 EVALI patients was a generic THC cartridge made by multiple unregulated manufacturers and sold on the black market.136The brand is Dank Vapes. See Jennifer Maloney and Daniela Hernandez, “Vaping’s Black Market Complicates Efforts to Combat Crises,” Wall Street Journal, October 6, 2019. On the basis of the evidence, the Centers for Disease Control and Prevention concludes that vitamin E acetate has been identified “as a primary cause of EVALI.”137See the CDC webpage cited in note 133.
While some public health officials seized upon the epidemic as evidence that vaping in general is deleterious to health, the official recommendations from the Centers for Disease Control and Prevention (as I write this chapter) are to avoid vaping THC, to avoid the additive vitamin E acetate, to be aware of “the wide range of health effects” associated with THC use, and to seek help for abuse of cannabis from a healthcare professional. In particular, the CDC specifically warns against returning to smoking instead of vaping for those who quit smoking or are trying to quit.
If we heavily regulate, tax, or ban e-cigarettes, what might be the unintended consequences?
Some of the potential unintended consequences of over-regulating e-cigarettes are similar to those discussed earlier for tobacco, while others differ. The tax equity issue because of the regressivity of excise taxation remains, although not to the same extent as for cigarette taxes, since it is not the case that lower-income individuals are more likely to vape than higher-income individuals.138A review of studies found that “no clear patterns emerged” in the relation between socioeconomic status and ecigarette usage, and that, if anything, income appears to be positively associated with use. See Greg Hartwell et al., “Ecigarettes and Equity: A Systematic Review of Differences in Awareness and Use between Sociodemographic Groups,” Tobacco Control 26, no. e2 (2017): e85–e91. The more important consideration concerns the health consequences of discouraging the use of a nicotine product at the lower end of the continuum of risk and the potential for black-market substitution.
The harm reduction (as opposed to the abstinence) approach to tobacco control views tobacco and nicotine-containing products as lying along a continuum of risk.139See, for example, David B. Abrams, “Promise and Peril of Ecigarettes: Can Disruptive Technology Make Cigarettes Obsolete?,” JAMA 311, no. 2 (2014): 135–36. Combustible products, most notably cigarettes, pose the greatest hazards, while nicotine replacement therapies are the least hazardous products. Some public health authorities embracing the harm reduction approach, perhaps most notably Public Health England, place e-cigarettes close to the low-risk end of the continuum. The key question for harm reduction is what will happen if e-cigarettes are banned, heavily taxed, or saddled with overly burdensome regulation? If more people continue to smoke instead of switching to vaping or quitting, then the evidence reviewed above indicates that it is highly likely that public health would suffer. Per-unit or ad valorem taxation of e-cigarettes may also encourage substitution toward products with higher concentrations of nicotine, which may increase health harms for youth.140As of early 2020, every state tax on ecigarettes is ad valorem: a specific tax per milliliter of eliquid or per cartridge, or a combination of the two; in particular, no state taxes the concentration of nicotine. National Conference of State Legislatures, “Ecigarette & Vaping Product Taxes,” April 6, 2020, https://www.ncsl.org/research/fiscal-policy/electronic-cigarette-taxation.aspx. On the potential for nicotine to harm the development of the adolescent brain, see note 147. On the other hand, if vaping renormalizes smoking and increases initiation among youth, public health could suffer in the future. (Discussion of these consequences continues in the next section.)
Given the relative novelty of vaping, illicit trade in e-cigarette products is much less studied than illicit trade in tobacco products.141For one of the rare examples of research on illicit trade in ecigarette products, see Prieger et al., Impact of Ecigarette Regulation. Apparently a thriving black market in counterfeit e-cigarettes already exists, although the prevalence is unknown and claims by manufacturers may be overstated. A worrisome feature of counterfeit eliquids is the uncertainty about what they contain; one study found that many of them contain nicotine even when they are labeled as zero-nicotine products.142See Esther E. Omaiye et al., “Counterfeit Electronic Cigarette Products with Mislabeled Nicotine Concentrations,” Tobacco Regulatory Science 3, no. 3 (2017): 347–57. Black-market THC vaping products have been found to contain pesticides, heavy metals, and lead, and counterfeit nicotine eliquids have been traced to illicit, unsanitary facilities in China.143See Maloney and Hernandez, “Vaping’s Black Market.” Packaging and supplies to assemble counterfeit vaping products are readily available online.143See Daniela Hernandez, “Sales of Illicit Vaping Products Find Home Online,” Wall Street Journal, September 20, 2019. The barriers to entry into the market for counterfeit products therefore seem to be low. As in any other market, as taxes or sales restrictions on licit products rise, substitution of illicit sources by some users should be expected, although the sensitivity to taxation of illicit trade in e-cigarette products has not been explored yet.
There is another important factor linking regulation of e-cigarettes to illicit trade, however. When e-cigarettes are readily available to smokers at reasonable prices, they offer smokers an attractive alternative to buying illicit tobacco products to reduce the costs of consuming nicotine. E-cigarettes could thus attenuate the link between higher cigarette taxes and stricter regulation of traditional tobacco products and ITTP. An econometric study found empirical support for this hypothesis.144See Prieger et al., Impact of Ecigarette Regulation. The study has not yet undergone peer review, however. Using data from Europe, econometric analysis showed that in places lacking availability of e-cigarettes, there was a sizeable, statistically significant positive relationship between tax increases for cigarettes and ITTP. However, the availability of e-cigarettes attenuated the size of that link: “the more available e-cigarettes become, the less the ITTP market share rises in response to tax-driven price increases for conventional cigarettes.”145Prieger et al., Impact of Ecigarette Regulation. In places where e-cigarette markets are large enough, cigarette prices no longer have any significant effect on illicit trade.
Steps toward Better Regulation
If more were understood about the actual health effects of vaping and exactly what the relationships are among the prices of tobacco and e-cigarettes, vaping, and youth initiation of smoking, and furthermore if society agreed that vapers and smokers need to be “saved from themselves” because of irrational choices, then in principal one could compute optimal prices for tobacco and e-cigarettes and levy taxes to achieve them. Complicating the analysis are the additional factors discussed above regarding the relationships among the price of tobacco, the price and attractiveness of vaping, and illicit trade. Furthermore, policymakers would also have to decide whether and how to weigh the equity considerations raised by tobacco taxation. Given the great uncertainty about the precise degree to which vaping is safer than smoking, no such tax rates can be computed at present. However, although a “first best” regulatory policy toward tobacco and vapor cannot be determined, there are sensible steps that can be taken that are likely to be in the right direction.
For tobacco, difficult and honest discussion needs to take place about the role of high rates of excise taxation. Given the evidence discussed above that current tax rates are higher than those required to correct for externalities and that the burden falls heavily on low-income individuals, the remaining rationales for taxation rest on paternalism, whether it is dressed in the clothing of behavioral economics or not.146“Government measures to reduce smoking through higher taxes would seem to be a form of paternalism about which economics has little to say.” Cnossen, “Tobacco Taxation in the European Union, p. 315.” How much of states’ and localities’ desire to tax tobacco stems from the ease of raising revenue from a socially disfavored minority?
Regarding e-cigarettes, the following seven recommendations can guide policymakers toward better regulation. First, the overriding principle that shapes thinking about regulating tobacco and e-cigarettes should be risk-proportionate regulation.147See Frank J. Chaloupka, David Sweanor, and Kenneth E. Warner, “Differential Taxes for Differential Risks—Toward Reduced Harm from Nicotine-Yielding Products,” New England Journal of Medicine 373, no. 7 (2015): 594–97. For discussion of proportionate regulation regarding ecigarettes, see also Prieger et al., Impact of Ecigarette Regulation. Products that are not as harmful to health as cigarettes should be regulated less stringently, taxed at lower levels, or even encouraged if they aid in cessation of tobacco use. By deeming e-cigarettes to be “tobacco products,” the FDA created a setting that prompted all the anti-tobacco crusading zeal to be indiscriminately directed at vaping as well. But since vaping is almost surely less harmful to health than smoking, the regulatory touch should also be lighter.
Second, the public health community in the United States needs to curb its tendency to understate the likely health benefits of switching from cigarettes to e-cigarettes. Sometimes this understatement happens because people confuse the absolute risk from vaping with the relative risk of vaping versus smoking, since the absolute risk is often characterized in more certain or inflated terms than the current body of scientific evidence warrants. Since e-cigarettes may cause some health harms (this argument runs), therefore vaping is no better than smoking. When anti-vaping advocates in the public health community take the uncertainty in the scientific literature as license to make statements implying that e-cigarettes could be comparably risky to cigarettes—or even more dangerous—their statements are technically true, since the long-term health effects of vaping are unknown. But they are also highly misleading.148See, for example, the statement that “we don’t know whether ecigarette use is as lethal as combustible cigarette use, less lethal than combustible cigarette use, or more lethal than combustible cigarette use,” by one public health researcher. Virginia Commonwealth University, “An Often-Made Claim that Ecigarettes are ‘95% Safer’ Is Not Valid,” news release, EurekAlert, January 8, 2020, https://www.eurekalert.org/pub_releases/2020-01/vcu-aoc010820.php.
Such statements have helped convince many members of the public to hold potentially dangerous attitudes about the relative health harms of smoking and vaping. Surveys indicate that today the majority of Americans believe e-cigarettes are just as harmful as cigarettes, and about 10 percent think that vaping is more dangerous than smoking.149Jidong Huang et al., “Changing Perceptions of Harm of Ecigarette vs Cigarette Use among Adults in 2 US National Surveys from 2012 to 2017,” JAMA 2, no. 3 (2019). Fewer than 3 percent of adults think that e-cigarettes are much less harmful than cigarettes.150See the data from the National Cancer Institute, HINTS: Health Information National Trends Survey, “Compared to Smoking Cigarettes, Would You Say That Electronic Cigarettes Are . . . ,” accessed October 9, 2020, https://hints.cancer.gov/view-questions-topics/question-details.aspx?nq=1&qid=1282. These negative perceptions of e-cigarettes have grown rapidly in recent years. This is concerning, given that the perceived risk of smoking relative to vaping is known to affect the decision to use e-cigarettes.151See, for example, Olivia A. Wackowski and Cristine D. Delnevo, “Young Adults’ Risk Perceptions of Various Tobacco Products Relative to Cigarettes: Results from the National Young Adult Health Survey,” Health Education and Behavior 43, no. 3 (2016): 328–36.
Third, the uncertainty regarding the health effects of e-cigarettes should not be used to discourage smokers from switching to vaping. The personal negative health impacts from smoking are large and well studied. Switching completely away from such a harmful activity to an activity that is very likely to be less harmful—even if the degree of relative risk is uncertain—is likely to improve the health prospects of the individual switching. The potential costs to public health of discouraging smokers from switching to e-cigarettes are high. One study found that, compared to the status quo, replacement of cigarette use by e-cigarette use over a 10-year period would result in 1.6–6.6 million fewer premature deaths and 20.8–86.7 million fewer years of life lost.152David T. Levy et al., “Potential Deaths Averted in USA by Replacing Cigarettes with Ecigarettes,” Tobacco Control 27, no. 1 (2018): 18–25.
Fourth, given the potential benefits to adult smokers from switching to e-cigarettes and the potential harms to youth from taking up vaping or, in consequence, smoking, targeting regulation narrowly at youth may be better than blunt, broadly applied rules. Thus the current age limits on purchases of e-cigarettes are mainly uncontroversial, as is the FDA’s enforcement against eliquids designed to resemble child-friendly food products. So would be, presumably, future restrictions on advertising aimed at youth. Of course, youth-oriented restrictions may prevent some young people who already smoke from switching to a less harmful product, since most current smokers began their habit before age 18. (As noted earlier, the age restriction for e-cigarette sales is now 21.)
Expending tobacco control funds on campaigns and information to alert youth to the potential dangers of vaping, in principle, is also relatively uncontroversial, since nicotine may have adverse health effects for adolescents that it does not have for adults.153The scientific evidence “is suggestive” that exposure to nicotine during adolescence may have “lasting adverse consequences for brain development,” resulting in adversely affected cognitive function and development. Health Consequences of Smoking—50 Years of Progress, 126. However, as with any abstinence campaign, it is likely that some youth will reject such messages, particularly if they sense that the claims are overblown or manipulative. Given the absence of solid knowledge about adverse health effects, some youth-oriented anti-vaping messages instead rely on false syllogisms along these lines: “Big Tobacco wants you to vape, and tobacco kills—therefore vaping will kill you.” Others attempt to parlay the recent epidemic of EVALI into messages not to use licit products such as JUUL and other commercially available, non-THC e-cigarettes, which does not appear to be a supportable conclusion (given the current but evolving knowledge reviewed earlier in this chapter).154For example, see the article for schoolchildren sponsored by the Centers for Disease Control and Prevention, part of its “The Real Cost” ecigarette prevention campaign: “The Health Impacts of Ecigarettes: Discover the Truth about How These Devices Can Harm You,” Scholastic, 2019, http://www.scholastic.com/youthvapingrisks/healthrisksofcigarettes_studentarticle_A.pdf. The article uses the EVALI cases to lead into the anti-ecigarette message, clearly wanting the reader to link those health harms with uses of any ecigarette. It is an open question why the same public health community that rejects fear-based anti-drug messages as ineffective or, worse, causing a boomerang effect155“We continue to be concerned that many of [the Office of National Drug Control Policy]’s advertisements are exaggerated fear appeals, which most experts in public health communications have concluded almost never work.” William Dejong and Lawrence Wallack, “The Drug Czar’s Anti-drug Media Campaign: Continuing Concerns,” Journal of Health Communication 5, no. 1 (2000): 77–82. See also the article cited by Dejong and Wallack: R. F. Soames Job, “Effective and Ineffective Use of Fear in Health Promotion Campaigns,” American Journal of Public Health 78, no. 2 (1988): 163–67. embraces them for the anti-vaping crusade.
Fifth, given the benefits of using regulation to target vaping by youth, heavily taxing e-cigarettes is not likely to be in the best interests of public health. As discussed previously, a tax (or any general regulation affecting all ages of users) is a very blunt instrument. While higher prices may deter some youth from using e-cigarettes, given the apparently large current appetite for black-market vapes that the EVALI epidemic revealed, coupled with the evidence from tobacco taxes and ITTP, it seems very likely that high taxes on e-cigarettes will drive more youth demand toward less reputable and potentially much more dangerous sources. In any event, sales to those under 21 years of age are already banned, which is equivalent to an infinitely high tax that applies only to youth. Furthermore, burdening adult smokers with high taxes will discourage some of them from switching to vaping, to the likely detriment of their health.
Indeed, if e-cigarettes are viewed as a form of nicotine-replacement therapy, there might even be a case for subsidizing them for smokers attempting cessation (as NRTs are subsidized through private health insurance and various public programs) rather than taxing them. Thus, proposed legislation such as the E-cigarette Tax Parity Act, which seeks to tax nicotine equally regardless of the mode of delivery, not only almost certainly violate the principle of risk-proportionate regulation but also may be harmful to public health.156Ecigarette Tax Parity Act, S. 2463, 116th Cong. (2019).
Sixth, careful consideration is warranted about whether banning the use of e-cigarettes in public spaces is appropriate. As reviewed above, it is far more certain that switching from smoking to vaping is beneficial for the health of the user than it is that e-cigarettes create substantial health harms from secondary exposure. But the ability to use e-cigarettes to consume nicotine, even if only in designated areas, while at work or in public spaces could be a powerful incentive for a smoker to switch. On the flip side, the ability to consume nicotine more easily may also prevent or delay some smokers from cessation (the “dual use” case). More study will be required to resolve these uncertainties, but it is not at all clear that excessive caution is better than cautious optimism regarding the social costs and benefits of vaping bans in public and work spaces. Banning vaping where smoking is banned also sends the message that the two activities are equally harmful, when they most likely are not—see again the second and third points discussed above.
Seventh, efforts to resolve the regulatory uncertainty at the federal level should be regarded as highly important. The FDA currently states that “no ENDS products have been authorized by the FDA—meaning that all ENDS products currently on the market are considered illegally marketed and are subject to enforcement, at any time, in the FDA’s discretion.”157See Food and Drug Administration, “FDA Finalizes Enforcement Policy on Unauthorized Flavored Cartridge-Based Ecigarettes That Appeal to Children, Including Fruit and Mint,” news release, January 2, 2020, https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children. Yet the agency has so far allowed sales of commercial nicotine e-cigarette products, as long as there are no sales or marketing to youth. The current regulatory environment is thus one in which the industry and the specific manufacturers and retailers in the industry are subject to a higher degree of regulatory dependence and uncertainty than affects most other industries. The negative effects of regulatory uncertainty and regulatory delay on investment and product innovation are well studied in other industries.158See, e.g., George Bittlingmayer, “Regulatory Uncertainty and Investment: Evidence from Antitrust Enforcement,” Cato Journal 20, no. 3 (2001): 295–326; James E. Prieger, “Regulation, Innovation, and the Introduction of New Telecommunications Services,” Review of Economics and Statistics 84, no. 4 (2002): 704–15; and Kira R. Fabrizio, “The Effect of Regulatory Uncertainty on Investment: Evidence from Renewable Energy Generation,” Journal of Law, Economics, and Organization 29, no. 4 (2013): 765–98. If e-cigarettes aid cessation or otherwise reduce harms from smoking, then innovation in that product space should be encouraged rather than discouraged.
Finally, in regard to both tobacco and e-cigarettes, policymakers must pay serious attention to the interplay among taxation, regulation, and illicit markets. If e-cigarettes are inexpensive, attractive to users, easy to obtain, and able to be used in places where smoking is forbidden, then current smokers will be less likely turn to the black market when they are faced with higher taxes on cigarettes or increased restrictions on smoking.159See Prieger et al., Impact of Ecigarette Regulation. See also the discussion in the previous section. Because the argument that higher taxes stimulate ITTP is convenient for tobacco manufacturers lobbying for lower tax rates, the public health community has a long history of discounting the possibility out of hand. This is despite the well-established links economists have found between cigarette taxation and smuggling.160See the discussion in the previous section. The already-present black market in tobacco, e-cigarettes, and eliquids should not be viewed as a theoretical possibility of limited practical import. Instead, illicit trade in all these product markets—and the likelihood that stricter regulation and higher taxation will exacerbate it—must be part of the policy calculus from the beginning.
Policymakers should plan for enforcement against illicit markets, and this enforcement must include action stronger than the tool currently preferred by the FDA—warning letters sent to noncompliant retailers and manufacturers.161See Food and Drug Administration, Enforcement Priorities for Electronic Nicotine Delivery Systems, § IV.E. Policymakers must also recognize that harsher, more effective enforcement can create its own harms—a notion familiar to the harm reduction community regarding illicit drugs, but curiously absent among anti-tobacco advocates.162For discussion with reference to drug markets, see Jonathan Caulkins and Peter Reuter, “Towards a Harm-Reduction Approach to Enforcement,” Safer Communities 8, no. 1 (2009): 9–23. For discussion with reference to tobacco markets, see Prieger, Kulick, and Kleiman, “Unintended Consequences of Cigarette Prohibition.”
References
83 Fed. Reg. 11818 (March 16, 2018).
83 Fed. Reg. 12294 (March 21, 2018).
83 Fed. Reg. 26618 (June 8, 2018).
“A State-by-State Look at the 1998 Tobacco Settlement 21 Years Later.” Campaign for Tobacco-Free Kids. Last modified January 16, 2020. https://www.tobaccofreekids.org/what-we-do/us/statereport.
Abrams, David B. “Promise and Peril of Ecigarettes: Can Disruptive Technology Make Cigarettes Obsolete?” JAMA 311. No. 2 (2014): 135–36.
Almond, Douglas, Kenneth Y. Chay, and David S. Lee. “The Costs of Low Birth Weight” Quarterly Journal of Economics 120. No. 3 (2005): 1031–83.
Apollonio, Dorie E. and Stanton A. Glantz. “Minimum Ages of Legal Access for Tobacco in the United States from 1863 to 2015.” American Journal of Public Health 106. No. 7 (2016): 1200–207.
Baker, Hannah M. et al. “Youth Source of Acquisition for Ecigarettes.” Preventive Medicine Reports 16 (2019).
Banderali, G. et al. “Short and Long Term Health Effects of Parental Tobacco Smoking during Pregnancy and Lactation: A Descriptive Review.” Journal of Translational Medicine 13 (2015).
Barrett, Malachi. “Michigan Senate Approves Ban on Ecigarette Sales to Minors.” MLive. April 23, 2019.
Bate, Roger, Cody Kallen, and Aparna Mathur. “The Perverse Effect of Sin Taxes: The Rise of Illicit White Cigarettes.” Applied Economics 52. No. 8 (2020): 789–805.
Bates, Clive. “Vaping Is Still at Least 95% Lower Risk than Smoking—Debunking a Feeble and Empty Critique.” The Counterfactual (blog). January 17, 2020.
Bates, Clive. “World Health Organisation Fails at Science and Fails at Propaganda—the Sad Case of WHO’s Anti-vaping Q&A.” The Counterfactual (blog). January 30, 2020.
Baugh, Janet G. et al. “Development Trends of First Cigarette Smoking Experience of Children: The Bogalusa Heart Study.” American Journal of Public Health 72. No. 10 (1982): 1161–64.
Becker, Gary S. and Kevin M. Murphy. “A Theory of Rational Addiction.” Journal of Political Economy 96. No. 4 (1988): 675–700.
Bennett, Oliver. “How Counterfeit Cigarettes Containing Pesticides and Arsenic Make It to Our Streets.” Independent. August 7, 2018.
Bittlingmayer, George. “Regulatory Uncertainty and Investment: Evidence from Antitrust Enforcement.” Cato Journal 20. No. 3 (2001): 295–326.
Blount, et al. “Vitamin E Acetate in Bronchoalveolar-Lavage Fluid Associated with EVALI.” New England Journal of Medicine 382. No. 8 (2020):697-705.
Bonnie, Richard J., Kathleen Stratton, and Leslie Y. Kwan, eds. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products (Washington, DC: National Academies Press. 2015).
Browning, Edgar K. “The Myth of Fiscal Externalities.” Public Finance Review 27. No. 1 (January 1999): 3–18.
Caulkins, Jonathan and Peter Reuter. “Towards a Harm-Reduction Approach to Enforcement.” Safer Communities 8. No. 1 (2009): 9–23.
Chaloupka, Frank J., David Sweanor, and Kenneth E. Warner. “Differential Taxes for Differential Risks—Toward Reduced Harm from Nicotine-Yielding Products.” New England Journal of Medicine 373. No. 7 (2015): 594–97.
Cheng, Tianrong. “Chemical Evaluation of Electronic Cigarettes.” Tobacco Control 23. No. S2 (2014): 11–17.
Cnossen, Sijbren. “Tobacco Taxation in the European Union.” FinanzArchiv/Public Finance Analysis 62. No. 2 (2006): 305–22.
Collins, Randall. “Tobacco Ritual and Anti-ritual: Substance Ingestion as a History of Social Boundaries.” in Interaction Ritual Chains (Princeton, NJ: Princeton University Press. 2004).
Colman, Gregory J. and Dahlia K. Remler. “Vertical Equity Consequences of Very High Cigarette Tax Increases: If the Poor Are the Ones Smoking, How Could Cigarette Tax Increases Be Progressive?” Journal of Policy Analysis and Management 27. No. 2 (2008): 376–400.
Creamer, MeLisa R. et al. “Tobacco Product Use and Cessation Indicators among Adults—United States, 2018.” Morbidity and Mortality Weekly Report 68. No. 45 (2019): 1013–19.
Crowley, George R. and Adam J. Hoffer. “Earmarking Tax Revenues: Leviathan’s Secret Weapon?” in Hoffer and Nesbit. For Your Own Good.
Cullen, Karen A. et al. “Ecigarette Use among Youth in the United States, 2019.” JAMA 322. No. 21 (2019): 2095–103.
Dave, Dhaval et al. “Does Ecigarette Advertising Encourage Adult Smokers to Quit?” Journal of Health Economics 68 (2019): 102227.
Dave, Dhaval, Bo Feng, and Michael F. Pesko. “The Effects of E-cigarette Minimum Legal Sale Age Laws on Youth Substance Use.” Health Economics 28. No. 3 (2019): 419–36.
DeCicca, Philip and Logan McLeod. “Cigarette Taxes and Older Adult Smoking: Evidence from Recent Large Tax Increases.” Journal of Health Economics 27. No. 4 (2008): 918–29.
DeCicca, Philip et al. “The Economics of Smoking Prevention.” in Oxford Research Encyclopedia of Economics and Finance (Oxford: Oxford University Press. 2018).
DeCicca, Philip et al. “Youth Smoking, Cigarette Prices, and Anti‐smoking Sentiment.” Health Economics 17. No. 6 (2007): 733–49.
DeCicca, Philip, Donald Kenkel, and Feng Liu. “Excise Tax Avoidance: The Case of State Cigarette Taxes.” Journal of Health Economics 32. No. 6 (2013): 1130–41.
Dejong and Wallack: R. F. Soames Job. “Effective and Ineffective Use of Fear in Health Promotion Campaigns.” American Journal of Public Health 78. No. 2 (1988): 163–67.
Dejong, William and Lawrence Wallack. “The Drug Czar’s Anti-drug Media Campaign: Continuing Concerns.” Journal of Health Communication 5. No. 1 (2000): 77–82.
Ecigarette Tax Parity Act. S. 2463. 116th Cong. (2019).
Eissenberg, Thomas et al. “Invalidity of an Oft-Cited Estimate of the Relative Harms of Electronic Cigarettes.” American Journal of Public Health 110. No. 2 (2020): 161–62.
El-Mohandes, Ayman et al. “An Intervention to Reduce Environmental Tobacco Smoke Exposure Improves Pregnancy Outcomes.” Pediatrics 125. No. 4 (2010): 721–28.
Etter, Jean-Francois. “Gateway Effects and Electronic Cigarettes.” Addiction 113. No. 10 (2018): 1776–83.
Euromonitor International. Tobacco in the United States. Country Report. January 2019. Passport.
Faber, Timor et al. “Effect of Tobacco Control Policies on Perinatal and Child Health: A Systematic Review and Meta-Analysis” The Lancet Public Health 2. No. 9 (2017): e420–37.
Faber, Timor et al. “Smoke-Free Legislation and Child Health” npj Primary Care Respiratory Medicine 26. art. No. 16067 (2016): 1–8.
Fabrizio, Kira R. “The Effect of Regulatory Uncertainty on Investment: Evidence from Renewable Energy Generation.” Journal of Law, Economics, and Organization 29. No. 4 (2013): 765–98.
Fairchild, Amy et al. “Evidence, Alarm, and the Debate over Ecigarettes.” Science 366. No. 6471 (December 2019): 1318–20.
Fang, Hanming and Dan Silverman. “Time‐Inconsistency and Welfare Program Participation: Evidence from the NLSY.” International Economic Review 50. No. 4 (2009): 1043–77.
Farhi, Emmanuel and Xavier Gabaix. “Optimal Taxation with Behavioral Agents.” American Economic Review 110. No. 1 (2020): 298–336.
Farrelly, M. C. et al. “The Effects of Higher Cigarette Prices on Tar and Nicotine Consumption in a Cohort of Adult Smokers.” Health Economics 13. No. 1 (2004): 49–58.
Farrelly, Matthew C. et al. “Response by Adults to Increases in Cigarette Prices by Sociodemographic Characteristics.” Southern Economic Journal 68. No. 1 (2001): 156–65.
Farrelly, Matthew C., James M. Nonnemaker, and Kimberly A. Watson. “The Consequences of High Cigarette Excise Taxes for Low-Income Smokers.” PLOS ONE 7. No. 9 (2012): e43838.
FDA v. Brown & Williamson Tobacco Corp. (98-1152). 529 U.S. 120 (2000). 153 F.3d 155. Affirmed.
Flue-Cured Tobacco Co-op. v. U.S.E.P.A. 4 F. Supp. 2d 435 (M.D.N.C. 1998). Flue-Cured Tobacco Cooperative Stabilization Co. et al. v. Environmental Protection Agency et al. 313 F.3d 852 (4th Cir. 2002).
Fong, Geoffrey T. et al. “The Near-Universal Experience of Regret among Smokers in Four Countries: Findings from the International Tobacco Control Policy Evaluation Survey.” Nicotine & Tobacco Research 6. No. 3 (2004): 341–51.
Food and Drug Administration. “FDA Finalizes Enforcement Policy on Unauthorized Flavored Cartridge-Based Ecigarettes That Appeal to Children, Including Fruit and Mint.” News release. January 2, 2020. https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children.
Food and Drug Administration. Enforcement Priorities for Electronic Nicotine Delivery Systems (ENDS) and Other Deemed Products on the Market without Premarket Authorization: Guidance for Industry. January 2020. https://www.fda.gov/media/133880/download.
Food and Drug Administration. Enforcement Priorities for Electronic Nicotine Delivery Systems.
Fox, Lindsay. “Smoking vs. Vaping: The Ultimate Cost Comparison.” EcigaretteReviewed (blog). February 25, 2016.
Friedman, A. S. “How Does Electronic Cigarette Access Affect Adolescent Smoking?” Journal of Health Economics 44 (2015): 300–308.
Fullerton, Don and Diane L. Rogers. Who Bears the Lifetime Tax Burden? (Washington, DC: Brookings Institution Press. 1993).
Glaeser, Edward L. “Paternalism and Psychology.” Regulation 29. No. 2 (2006).
Glass, Andrew. “Congress Bans Airing Cigarette Ads, April 1, 1970.” Politico. April 1, 2018.
Goel, Rajiv and James W. Saunoris. “Cigarette Smuggling: Using the Shadow Economy or Creating Its Own?” Journal of Economics and Finance 43 (2019): 582–93.
Gravell, Jane G. and Dennis Zimmerman. Cigarette Taxes to Fund Health Care Reform: An Economic Analysis (Washington, DC: Library of Congress. 1994).
Green, Lawrence W., Jonathan E. Fielding, and Ross C. Brownson. “The Debate about Electronic Cigarettes: Harm Minimization or the Precautionary Principle.” Annual Review of Public Health 39 (2018): 189–91.
Gruber, Jonathan and Botond Köszegi. A Modern Economic View of Tobacco Taxation (Paris: International Union against Tuberculosis and Lung Disease. 2008).
Gruber, Jonathan. Public Finance and Public Policy (New York: Worth Publishers, 2005). 547.
Hajek, Peter et al. “A Randomized Trial of Ecigarettes versus Nicotine-Replacement Therapy.” New England Journal of Medicine 380 (2019): 629–37.
Hammond, David et al. “Text and Graphic Warnings on Cigarette Packages: Findings from the International Tobacco Control Four Country Study.” American Journal of Preventive Medicine 32. No. 3 (2007): 202–9.
Hartwell, Greg et al. “Ecigarettes and Equity: A Systematic Review of Differences in Awareness and Use between Sociodemographic Groups.” Tobacco Control 26. No. e2 (2017): e85–e91.
Health Consequences of Smoking—50 Years of Progress. 126.
Health Information National Trends Survey. “Compared to Smoking Cigarettes, Would You Say That Electronic Cigarettes Are . . . ” Accessed October 9, 2020. https://hints.cancer.gov/view-questions-topics/question-details.aspx?nq=1&qid=1282.
Henriksen, Lisa et al. “Assurances of Voluntary Compliance: A Regulatory Mechanism to Reduce Youth Access to Ecigarettes and Limit Retail Tobacco Marketing.” American Journal of Public Health 110. No. 2 (2020): 209–15.
Hernandez, Daniela. “Sales of Illicit Vaping Products Find Home Online.” Wall Street Journal. September 20, 2019.
Heron, Melanie. “Deaths: Leading Causes for 2014.” National Vital Statistics Reports 65. No. 5 (2016): 1–95.
Hess, Isabel M. R., Kishen Lachireddy, and Adam Capon. “A Systematic Review of the Health Risks from Passive Exposure to Electronic Cigarette Vapour.” Public Health Research and Practice 26. No. 2 (2016).
Hiilamo, Heikki, Eric Crosbie, and Stanton A. Glantz. “The Evolution of Health Warning Labels on Cigarette Packs: The Role of Precedents, and Tobacco Industry Strategies to Block Diffusion.” Tobacco Control 23. No. 1 (2014): e2.
Hoffer, Adam J. and Todd Nesbit, eds. For Your Own Good: Taxes, Paternalism, and Fiscal Discrimination in the Twenty-First Century (Arlington, VA: Mercatus Center at George Mason University. 2018).
Hoffer, Adam J., William F. Shughart II, and Michael D. Thomas. “Sin Taxes and Sindustry: Revenue, Paternalism, and Political Interest.” Independent Review 19. No. 1 (2014): 47–64.
Huang, Jidong et al. “Changing Perceptions of Harm of Ecigarette vs Cigarette Use among Adults in 2 US National Surveys from 2012 to 2017.” JAMA 2. No. 3. (2019).
Huber, Gary L., Robert E. Brockie, and Vijay K. Majhajan. “Smoke and Mirrors: The EPA’s Flawed Study of Environmental Tobacco Smoke and Lung Cancer.” Regulation 16. No. 3 (1993): 44–54.
“Increases and Changes to Consumer Taxes in Chicago for 2020.” Civic Federation. January 10, 2020. https://www.civicfed.org/civic-federation/blog/increases-and-changes-consumer-taxes-chicago-2020.
Institute of Medicine. Ending the Tobacco Problem: A Blueprint for the Nation. Ed. Richard J. Bonnie, Kathleen Stratton, and Robert B. Wallace (Washington, DC: National Academies Press. 2007).
Joossens, Luk and Martin Raw. “From Cigarette Smuggling to Illicit Tobacco Trade.” Tobacco Control 21. No. 2 (2012): 230–34.
Kabat, G. C. “Fifty Years’ Experience of Reduced-Tar Cigarettes: What Do We Know about Their Health Effects?” Inhalation Toxicology 15. No. 11 (2003): 1059–102.
Kenneth Warner et al. “Criteria for Determining an Optimal Cigarette Tax: The Economist’s Perspective.” Tobacco Control 4. No. 4 (1995): 380–86.
Ko, Ting-Jung et al. “Parental Smoking during Pregnancy and Its Association with Low Birth Weight, Small for Gestational Age, and Preterm Birth Offspring: A Birth Cohort Study.” Pediatrics and Neonatology 55. No.1 (2014): 20–27.
Kozlowski, Lynn T. and Kenneth E. Warner. “Adolescents and Ecigarettes: Objects of Concern May Appear Larger Than They Are.” Drug and Alcohol Dependence 174 (2017): 209–14.
LaFaive, Michael. “Prohibition by Price: Cigarette Taxes and Unintended Consequences.” in Hoffer and Nesbit. For Your Own Good.
LaVito, Angelica. “CDC Says Teen Vaping Surges to More than 1 in 4 High School Students.” CNBC. September 12, 2019.
Levy, D. T. et al. “Examining the Relationship of Vaping to Smoking Initiation among US Youth and Young Adults: A Reality Check.” Tobacco Control 28. No. 6 (2019): 629–35.
Levy, David T. et al. “Potential Deaths Averted in USA by Replacing Cigarettes with Ecigarettes.” Tobacco Control 27. No. 1 (2018): 18–25.
Lillard, Dean R., Eamon Molloy, and Andrew Sfekas. “Smoking Initiation and the Iron Law of Demand.” Journal of Health Economics 32. No. 1 (2013): 114–27.
Lyon, Andrew B. and Robert M. Schwab. “Consumption Taxes in a Life-Cycle Framework: Are Sin Taxes Regressive?” Review of Economics and Statistics 77. No. 3 (1995): 389–406.
Maloney, Jennifer and Daniela Hernandez. “Vaping’s Black Market Complicates Efforts to Combat Crises.” Wall Street Journal. October 6, 2019.
Maloney, Jennifer. “FDA Clears Philip Morris International Heat-Not-Burn IQOS Device for Sale in U.S.” Wall Street Journal. April 30, 2019.
Manning, Willard G. et al. “The Taxes of Sin: Do Smokers and Drinkers Pay Their Way?” JAMA 261. No. 11 (1989): 1604–9.
Marlow, Michael L. and Sherzod Abdukadirov. “Taxation as Nudge: The Failure of Anti-obesity Paternalism.” in Hoffer and Nesbit. For Your Own Good.
McConnell, Rob et al. “Electronic Cigarette Use and Respiratory Symptoms in Adolescents,” American Journal of Respiratory and Critical Care Medicine 195. No. 8 (2017): 1043–49.
McGeary, Kerry Anne et al. “Impact of Comprehensive Smoking Bans on the Health of Infants and Children.” American Journal of Health Economics 6. No. 1 (2020): 1–38.
McNeill, A. et al. Ecigarettes: An Evidence Update (London: Public Health England. 2015).
Moran, Lee. “Fake Cigarettes Containing Human Feces, Rat Droppings Flood British Market: Report.” New York Daily News. November 11, 2014.
“NAAG Center for Tobacco and Public Health.” National Association of Attorneys General. Accessed July 2, 2020. https://www.naag.org/naag/about_naag/naag-center-for-tobacco-and-public-health.php.
Naimi, Timothy S. et al. “Erosion of State Alcohol Excise Taxes in the United States.” Journal of Studies on Alcohol and Drugs 79. No. 1 (2018): 43–48.
National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of Ecigarettes (Washington, DC: National Academies Press. 2018).
National Conference of State Legislatures. “Ecigarette & Vaping Product Taxes.” April 6, 2020. https://www.ncsl.org/research/fiscal-policy/electronic-cigarette-taxation.aspx.
National Research Council and Institute of Medicine. Understanding the U.S. Illicit Tobacco Market: Characteristics, Policy Context, and Lessons from International Experiences. Ed. Peter Reuter and Malay Majmundar (Washington, DC: National Academies Press. 2015). 4.
Noar, Seth M. et al. “Pictorial Cigarette Pack Warnings: A Meta-analysis of Experimental Studies.” Tobacco Control 25. No. 3 (2016): 341–54.
Omaiye, Esther E. et al. “Counterfeit Electronic Cigarette Products with Mislabeled Nicotine Concentrations.” Tobacco Regulatory Science 3. No. 3 (2017): 347–57.
Outbreak of Lung Injury Associated with the Use of Ecigarette, or Vaping, Products.” Accessed October 9, 2020. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
Pepper, Jessica K. et al. “How Do Adolescents Get Their Ecigarettes and Other Electronic Vaping Devices?” American Journal of Health Promotion 33. No. 3 (2019).
Pesko, Michael F. and Janet M. Currie. “Ecigarette Minimum Legal Sale Age Laws and Traditional Cigarette Use among Rural Pregnant Teenagers.” Journal of Health Economics 66 (2019): 71–90.
Prieger, James and Jonathan Kulick. “Unintended Consequences of Enforcement in Illicit Markets.” Economics Letters 125. No. 2 (2014): 295–97.
Prieger, James E. “Regulation, Innovation, and the Introduction of New Telecommunications Services.” Review of Economics and Statistics 84. No. 4 (2002): 704–15.
Prieger, James E. and Jonathan Kulick. “Cigarette Taxes and Illicit Trade in Europe.” Economic Inquiry 56. No. 3 (2018): 1706–23.
Prieger, James E. and Jonathan Kulick. “Tax Evasion and Illicit Cigarettes in California: Part IV—Smokers’ Behavioral and Market Responses to a Tax Increase.” BOTEC Analysis. January 24, 2019. https://ssrn.com/abstract=3322095.
Prieger, James E. and Jonathan Kulick. “Violence in Illicit Markets: Unintended Consequences and the Search for Paradoxical Effects of Enforcement.” B.E. Journal of Economic Analysis and Policy 15. No. 3 (2015): 1263–95.
Prieger, James E. et al. The Impact of Ecigarette Regulation on the Illicit Trade in Tobacco Products in the European Union (Geneva, Switzerland: BOTEC Analysis. 2019).
Prieger, James E., Jonathan Kulick, and Mark A. R. Kleiman. “Unintended Consequences of Cigarette Prohibition, Regulation, and Taxation.” International Journal of Law, Crime and Justice 46 (2016): 69–85.
Rahman, Muhammad Aziz et al. “Ecigarettes and Smoking Cessation: Evidence from a Systematic Review and Meta-analysis.” PLOS ONE 10. No. 3 (2015).
Regulations Restricting the Sale and Distribution of Cigarettes and Smokeless Tobacco to Protect Children and Adolescents. 75 Fed. Reg. 13225 (March 19, 2010).
Remler, Dahlia K. “Poor Smokers, Poor Quitters, and Cigarette Tax Regressivity.” American Journal of Public Health 94. No. 2 (2004): 225–29.
Required Warning Statement Regarding Addictiveness of Nicotine. 21 C.F.R. 1143.3 (April 1, 2019).
Rhee, Jongeun et al. “Maternal Caffeine Consumption during Pregnancy and Risk of Low Birth Weight: A Dose-Response Meta-analysis of Observational Studies.” PLOS ONE 10. No. 7 (2015): 1–18.
Rigotti, Nancy A. “Youth Access to Tobacco.” Nicotine and Tobacco Research 1, suppl. 2 (1999): S93–S97.
Ritter, Alison and Jacqui Cameron. “A Review of the Efficacy and Effectiveness of Harm Reduction Strategies for Alcohol, Tobacco and Illicit Drugs.” Drug and Alcohol Review 25. No. 6 (2006): 611–24.
Romer, Daniel and Patrick Jamieson. “Do Adolescents Appreciate the Risks of Smoking? Evidence from a National Survey.” Journal of Adolescent Health 29. No. 1 (2001): 12–21.
Ross, Hana and Frank J. Chaloupka. “The Effect of Cigarette Prices on Youth Smoking.” Health Economics 12. No. 3 (2003): 217–30.
Saffer, Henry et al. “Ecigarettes and Adult Smoking: Evidence from Minnesota” (NBER Working Paper No. 26589. National Bureau of Economic Research. Cambridge, MA. December 2019).
Salmasi, Giselle et al. “Environmental Tobacco Smoke Exposure and Perinatal Outcomes: A Systematic Review and Meta‐analyses.” Acta Obstetricia et Gynecologica Scandinavica 89. No. 4 (2010): 423–41.
Shahab, Lion et al. “Nicotine, Carcinogen, and Toxin Exposure in Long-Term Ecigarette and Nicotine Replacement Therapy Users: A Cross-Sectional Study.” Annals of Internal Medicine 166. No. 6 (2017): 390–400.
Sharpless, Ned. “How FDA Is Regulating Ecigarettes.” Food and Drug Administration. September 10, 2019. https://www.fda.gov/news-events/fda-voices-perspectives-fda-leadership-and-experts/how-fda-regulating-e-cigarettes.
Shelton, D. M. et al. “State Laws on Tobacco Control—United States, 1995.” Morbidity and Mortality Weekly Report Surveillance Summaries 44. No. 6 (1995): 1–28.
Simon, Michele. “Reducing Youth Exposure to Alcohol Ads: Targeting Public Transit.” Journal of Urban Health 85. No. 4 (2008): 506–16.
Smith, Julia, Sheryl Thompson, and Kelley Lee. “Death and Taxes: The Framing of the Causes and Policy Responses to the Illicit Tobacco Trade in Canadian Newspapers.” Cogent Social Sciences 3. No. 1 (2017).
Sobel, Russell S. and Joshua C. Hall. “In Loco Parentis: A Paternalism Ranking of the States.” in For Your Own Good: Taxes, Paternalism, and Fiscal Discrimination in the Twenty-First Century. Ed. Adam J. Hoffer and Todd Nesbit (Arlington, VA: Mercatus Center at George Mason University. 2018).
“State-by-State Look.” Campaign for Tobacco-Free Kids.
Stephens, W. Edryd, Angus Calder, and Jason Newton. “Source and Health Implications of High Toxic Metal Concentrations in Illicit Tobacco Products.” Environmental Science and Technology 39. No. 2 (2005): 479–88.
Stephens, William E. “Comparing the Cancer Potencies of Emissions from Vapourised Nicotine Products Including Ecigarettes with Those of Tobacco Smoke.” Tobacco Control 27. No. 1 (2018): 10–17.
Tanski, Susanne et al. “Youth Access to Tobacco Products in the United States: Findings from Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health Study.” Nicotine and Tobacco Research 2. No. 12 (December 2019): 1695–99.
The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General (Atlanta: US Department of Health and Human Services. 2014).
“The Health Impacts of Ecigarettes: Discover the Truth about How These Devices Can Harm You.” Scholastic. 2019. http://www.scholastic.com/youthvapingrisks/healthrisksofcigarettes_studentarticle_A.pdf.
The Tax Burden on Tobacco: Historical Compilation (Arlington, VA: Orzechowski and Walker. 2014).
Tobacco Products; Required Warnings for Cigarette Packages and Advertisements. 84 Fed. Reg. 42754 (August 16, 2019).
Tobacco Products; Required Warnings for Cigarette Packages and Advertisements. 85 Fed. Reg. 15638 (March 18, 2020).
Tobacco Regulation for Substance Abuse Prevention and Treatment Block Grants. 61 Fed. Reg. 1492 (January 19, 1996).
US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service (Washington, DC: US Government Printing Office. 1964). 32.
Vijayaraghavan, Maya et al. “The Effectiveness of Cigarette Price and Smoke-Free Homes on Low-Income Smokers in the United States.” American Journal of Public Health 103. No. 12 (2013): 2276–83.
Villanti, Andrea C. et al. “How Do We Determine the Impact of E‐cigarettes on Cigarette Smoking Cessation or Reduction? Review and Recommendations for Answering the Research Question with Scientific Rigor.” Addiction 113. No. 3 (2018): 391–404.
Virginia Commonwealth University. “An Often-Made Claim that Ecigarettes are ‘95% Safer’ Is Not Valid.” News release. EurekAlert. January 8, 2020. https://www.eurekalert.org/pub_releases/2020-01/vcu-aoc010820.php.
Viscusi, W. Kip. “The New Cigarette Paternalism.” Regulation 25. No. 4 (2002): 58–64.
Wackowski, Olivia A. and Cristine D. Delnevo. “Young Adults’ Risk Perceptions of Various Tobacco Products Relative to Cigarettes: Results from the National Young Adult Health Survey.” Health Education and Behavior 43 .No. 3 (2016): 328–36.
Warner et al. “Criteria for Determining an Optimal Cigarette Tax.”
Wasserman, Jeffrey et al. “The Effects of Excise Taxes and Regulations on Cigarette Smoking.” Journal of Health Economics 10. No. 1 (1991): 43–64.
Weaver, Scott R. et al. “Use of Electronic Nicotine Delivery Systems and Other Tobacco Products among USA Adults, 2014: Results from a National Survey.” International Journal of Public Health 61. No. 2 (2016): 177–88.
West, Robert, Jamie Brown, and Martin Jarvis. “Epidemic of Youth Nicotine Addiction? What Does the National Youth Tobacco Survey Reveal about High School Ecigarette Use in the USA?” Qeios preprint. Submitted October 7, 2019.
Wolff-Mann, Ethan. “Vaping Is 95% Healthier and 40% Cheaper Than Smoking.” Money. August 20, 2015.
World Health Organization. “Q&A Detail: Ecigarettes.” Accessed January 23, 2020. https://www.who.int/news-room/q-a-detail/e-cigarettes-how-risky-are-they.
Table of Contents
- Regulation and Entrepreneurship: Theory, Impacts, and Implications
- Regulation and the Perpetuation of Poverty in the US and Senegal
- Social Trust and Regulation: A Time-Series Analysis of the United States
- Regulation and the Shadow Economy
- An Introduction to the Effect of Regulation on Employment and Wages
- Occupational Licensing: A Barrier to Opportunity and Prosperity
- Gender, Race, and Earnings: The Divergent Effect of Occupational Licensing on the Distribution of Earnings and on Access to the Economy
- How Can Certificate-of-Need Laws Be Reformed to Improve Access to Healthcare?
- Land Use Regulation and Housing Affordability
- Building Energy Codes: A Case Study in Regulation and Cost-Benefit Analysis
- The Tradeoffs between Energy Efficiency, Consumer Preferences, and Economic Growth
- Cooperation or Conflict: Two Approaches to Conservation
- Retail Electric Competition and Natural Monopoly: The Shocking Truth
- Governance for Networks: Regulation by Networks in Electric Power Markets in Texas
- Net Neutrality: Internet Regulation and the Plans to Bring It Back
- Unintended Consequences of Regulating Private School Choice Programs: A Review of the Evidence
- “Blue Laws” and Other Cases of Bootlegger/Baptist Influence in Beer Regulation
- Smoke or Vapor? Regulation of Tobacco and Vaping
- Moving Forward: A Guide for Regulatory Policy