1. Introduction
Suicide is one of the leading causes of death in the United States (CDC, 2020). It is the second leading cause of death among individuals between the ages of 15 to 34. Over the past two decades, mortality resulting from suicide increased in nearly all 50 states and the District of Columbia. Over 44,000 lives were lost to suicide in 2016 alone (CDC, 2018). While there are many factors responsible for a person taking their own life, several studies have found strong associations between mental health issues and risk of suicide, with depression being ranked as the most prevalent catalyst (Arsenault-Lapierre et al., 2004; Bachmann, 2018; Brådvik, 2018; Chesney et al., 2014; Too et al., 2019). Improved access to mental healthcare might mitigate the “deaths of despair” and save some lives. Access problems are further highlighted by looking at the higher rates of suicide in rural areas underserved by healthcare providers (Bureau of Health Workforce, 2016).
In the United States, there can often be weeks or months between the time a psychologist identifies that a patient needs pharmacological intervention and when that patient is able to be seen, assessed, and given treatment by a separate psychiatrist. Those weeks or months can be a matter of life or death for individuals with suicidal intentions and expanding psychologist prescriptive authority reduces this time delay. Within this study, we investigate the effect of this prescriptive authority expansion on the most severe potential mental and behavioral health outcome, suicide.
We use restricted mortality data provided through the National Center for Health Statistics to analyze the impact on suicide rates of allowing psychologists prescriptive authority. Prescriptive authority means that, after meeting training, education, and experience requirements, psychologists can prescribe mental and behavioral health medication that they deem beneficial for the individual. Prescriptive authority is one of two types of scope-of-practice regulations within the medical field, the other being practice authority. In economics, several studies have linked scope-of-practice regulations to limits in access to healthcare services. Most studies focus on changes in practice authority, identifying changes in autonomy over job responsibilities. Within our study, psychologist autonomy in patient care did not change; instead the legal change was with the expansion of the right to prescribe medication. This is a unique addition to the literature since it explores one of the few policy vehicles that target prescriptive rather than practice authority.
Access problems can occur because of higher prices of healthcare services due to restrictive scope-of-practice laws (Kleiner et al., 2016; Kleiner & Park, 2010; Timmons & Norris, 2018). Most papers studying scope-of-practice laws focus on dental services (Kleiner & Park, 2010; Kleiner et al., 2016; Langelier et all, 2016), primary care vs. nurse practitioners (Dueker et al., 2005; Stange, 2014; Xue et al., 2016; Traczysnki & Udalova, 2018), and physician assistants (Timmons, 2017). Our paper instead focuses on mental healthcare and suicide through psychologist scope of practice in terms of prescriptive authority, a market that has not been studied thoroughly in the literature.
The Prescription Privileges movement (hereafter RxP movement) is an ongoing policy debate that seeks to expand scope-of-practice privileges for psychologists to prescribe controlled substances. Mental healthcare services usually take two fundamental and often complementary forms: psychotherapy (such as talk therapy) and psychotropic medication. Allowing psychologists to prescribe psychotropic medication may increase access to treatment, particularly for disadvantaged or minority populations. Currently, there are five states where prescriptive authority exists: New Mexico (since 2002), Louisiana (since 2004), Illinois (since 2014), Iowa (since 2016), and Idaho (since 2017) (Alexander & Schnell, 2019). States that allow prescriptive privilege to psychologists require them to complete additional training, education, and experience requirements in psychopharmacology. These requirements create a substantial lagged effect between when a policy is passed and when psychologists are first able to prescribe psychotropic medications to patients.
Proponents of the RxP movement argue that allowing psychologists to prescribe controlled substances will improve access to mental healthcare services. Opponents of the policy state that quality of care will be poor, and patients may be prescribed inappropriate amounts of medication for their diagnoses. Existing literature in occupational licensing and scope of practice suggest mixed results on quality metrics for reductions in regulatory barriers, with some studies recording improvements due to better access to care. Our paper contributes to this research by analyzing how mortality due to suicides is affected by mental healthcare access by allowing psychologists to prescribe controlled substances. We use a difference-in-difference estimation strategy to determine whether prescription privileges for psychologists mitigate suicide deaths in states allowing prescriptive authority relative to others. We find that, in the long term, states with prescriptive authority have a reduction in suicides for men, women, Black, White, middle-aged, single, and divorced subpopulations.
The rest of the paper is organized as follows. Section 2 describes how our study fits with the existing literature and highlights our main contributions. Section 3 provides the methodology used in the paper while Section 4 describes the data sets used for our analysis. We present the results from our findings in Section 5 and provider the conclusion in Section 6.
2. Literature Review
Scope-of-practice regulations refer to state-level laws that dictate what types of specific procedures can or cannot be performed by healthcare providers. There are significant variations in scope-of-practice regulations across states, and across healthcare professions such as nurse practitioners, physician assistants, and pharmacists (McMichael, 2017; Stein et al., 2017). For instance, nurse practitioners in Alabama must collaborate under a supervising physician before they can order diagnostic tests. However, nurse practitioners in New Mexico do not need to collaborate with physicians, can order tests, and have prescriptive authority to prescribe medication without physician oversight (AANP, 2016).
Proponents state that scope-of-practice regulations promote better quality healthcare services and protection of physicians, who have invested more years to receive their degree. They also state that relaxing scope-of-practice laws might lead to overutilization of diagnostic testing (such as CT scan or MRI) and lead to higher healthcare costs and adverse health outcomes (Hughes et al., 2015). Regarding mental healthcare, this would translate to overprescribing psychotropic medications, which has a higher potential of being abused (Kaminer et al., 2010; Mamat et al., 2015). Regardless of the severity of scope-of-practice restrictions within a state, these restrictions are designed and implemented by state-based agencies such as the board of medicine, board of pharmacy, and the board of nursing (Phillips et al., 2014). These regulatory boards often include politicians, active members of the profession, and persons who have a vested interested in healthcare training schools (Slivinski, 2020).
However, opponents state that these regulations act as strong barriers to the provision of healthcare services, particularly for disadvantaged and rural residents (Federal Trade Commission, 2014). They also argue that restrictive scope-of-practice regulations cause higher healthcare costs by limiting the supply of healthcare services, which results in longer wait times and poorer long-term health outcomes (Kandrack et al., 2019). Most of the research regarding changes in scope-of-practice laws have focused on the responsibilities of nurse practitioners, pharmacists, dental hygienists, dental assistants, and physician assistants.
The literature has found evidence suggesting improved access, increased utilization of healthcare services (Timmons & Norris, 2018; Chen et al., 2020; Swan et al., 2015), and lower prices of healthcare services for customers after scope of practice is expanded to other providers (Kleiner et al., 2016; Kleiner & Park, 2010; Timmons & Norris, 2018).
Access can be especially difficult for mental and behavioral health services because there may be disparities in the willingness of insurance companies to cover this type of care due to parity laws. Lang (2013) finds that mental health parity laws can make it easier for people to access mental healthcare by structuring prices in a way that is more affordable within insurance coverage. Scope-of-practice regulations can also exacerbate the provider shortage crisis prevalent in healthcare today—for mental health services alone, there is a shortage of over 6,000 providers (HRSA, 2021).
Other studies have analyzed the availability of healthcare providers for catering to mental health patients on suicide rates. Multiple studies have found that areas with higher availability of healthcare providers, such as psychiatrists, physicians, and counselors, are associated with lower suicide rates. Tondo et al. (2006) find that higher density of psychiatrists and nonpsychiatrist physicians are associated with lower suicide rates. A different study using data from CDC finds that states with higher proportions of psychiatrists, psychologists, and social workers have lower suicide rates (Thomson Healthcare, 2007). Both studies rely on bivariate analysis, making it difficult to establish a strong causal association because there might be factors that affect both mental health outcomes and availability of providers.
Another variable used by researchers to capture access to mental healthcare services is distance to the nearest provider. McCarthy et al. (2012) study the distance to the nearest Veterans Affairs (VA) mental health provider as a factor affecting risk of suicides for active-duty military veterans. Controlling for sociodemographic factors and mental health diagnosis, the authors do not find any evidence suggesting that distance to the nearest VA is a strong predictor of suicide within this population. They only find a significant result for distances greater than 800 miles. However, they do not capture how distance affects lack of visits to a mental health provider in the VA.
Researchers have also found a strong link between federal mental health aid received by states and lower suicide rates. Tondo et al. (2006) find that states receiving more federal mental health aid have lower suicide rates. Their paper finds that federal mental health aid provided to states is a stronger predictor of overall state suicide rates than density of mental healthcare providers or proportion of uninsured individuals. There is also the issue of individuals with suicidal tendencies seeking therapy and treatment, and how successful these treatment methods are. Most mental health treatment is long term, requiring regular meetings and medication for months, years, or continuously. Niederkrotenthaler et al. (2014) use data on individuals that died by suicide between 2005 and 2010 to study the utilization of mental health services prior to death. They find that 38.5% suicide decedents had received mental health care within the previous two months before their death.
There are fewer studies analyzing the impact of scope-of-practice regulations on mental and behavioral healthcare access. In the study most similar to our own, Alexander and Schnell (2019) find that expanding independent scope of practice for nurse practitioners to prescribe controlled substances improves access to mental healthcare and reduces mental health related mortality, including suicides. This is the only study to the best of our knowledge that looks at how expansion of scope of practice affects mental healthcare outcomes. Furthermore, they find that the impact is greater on areas that are underserved, such as rural or minority communities. Our paper differs from theirs in that we focus on expansion of prescription authority specifically for psychologists instead of nurse practitioners, and we then determine how this expansion affects suicide-related mortality. We also make a detailed analysis of how expansion of prescriptive authority affects different groups of people by performing a subsample analysis. Other papers have also found that expanded scope of practice for nurse practitioners might help alleviate disparities in access to mental healthcare services (Bishop et al., 2014; Hartley et al., 2004; Traczynski & Udalova, 2018).
3. Data
To understand the ramifications of prescriptive authority on mental health outcomes, we focus on suicide rates within treated and untreated states before and after prescriptive authority for psychologists was implemented. Though deaths resulting from suicide can have many underlying factors, it is firmly associated as a mental and behavioral health outcome on which prescriptive medication has substantial mitigating effects (Gibbons et al., 2005; Olfson et al., 2003). We use mortality data (multiple cause of death) from the National Vital Statistics System of the National Center for Health Statistics for years 1999–2018 to analyze changes in deaths due to suicide.1We had access to the public data from 1996–2004 from the NBER website. However, NBER discontinued posting geographic identifiers from 2005. We had to apply to NCHS to receive the restricted version of the data set from 2005–2018. Data are aggregated to the state level to comply with restricted data reporting requirements. This data set contains information on all deaths occurring in the United States and contains categorical information on the cause(s) of death. This information is obtained from death certificates provided through vital statistics offices in all 50 states and the District of Columbia.
We restrict our analysis to include only deaths due to suicide for individuals over the age of 15. We aggregate the data set at the state, month, and year levels to include the number of deaths due to suicide in each month and year for a select state. Observations are aggregated to the state level within months to comply with the disclosure rules outlined in our data usage agreement. We do not report on some age categories above 64 or for some minority populations for lack of robust sample size to comply with the legal requirement. We then include information on the sex of individuals who died by suicide in each state at a given time. We add similar information regarding resident status, education level (high school, some college, bachelors, graduate), marital status (divorced, widowed, single, married), age group (multiple 10-year age intervals), and unemployment rate in the given state during a given month. Therefore, we have both observations of the aggregate number of deaths by suicide in a certain state at a certain time, as well as the different characteristics of people who died by suicide in a certain state at a certain time.
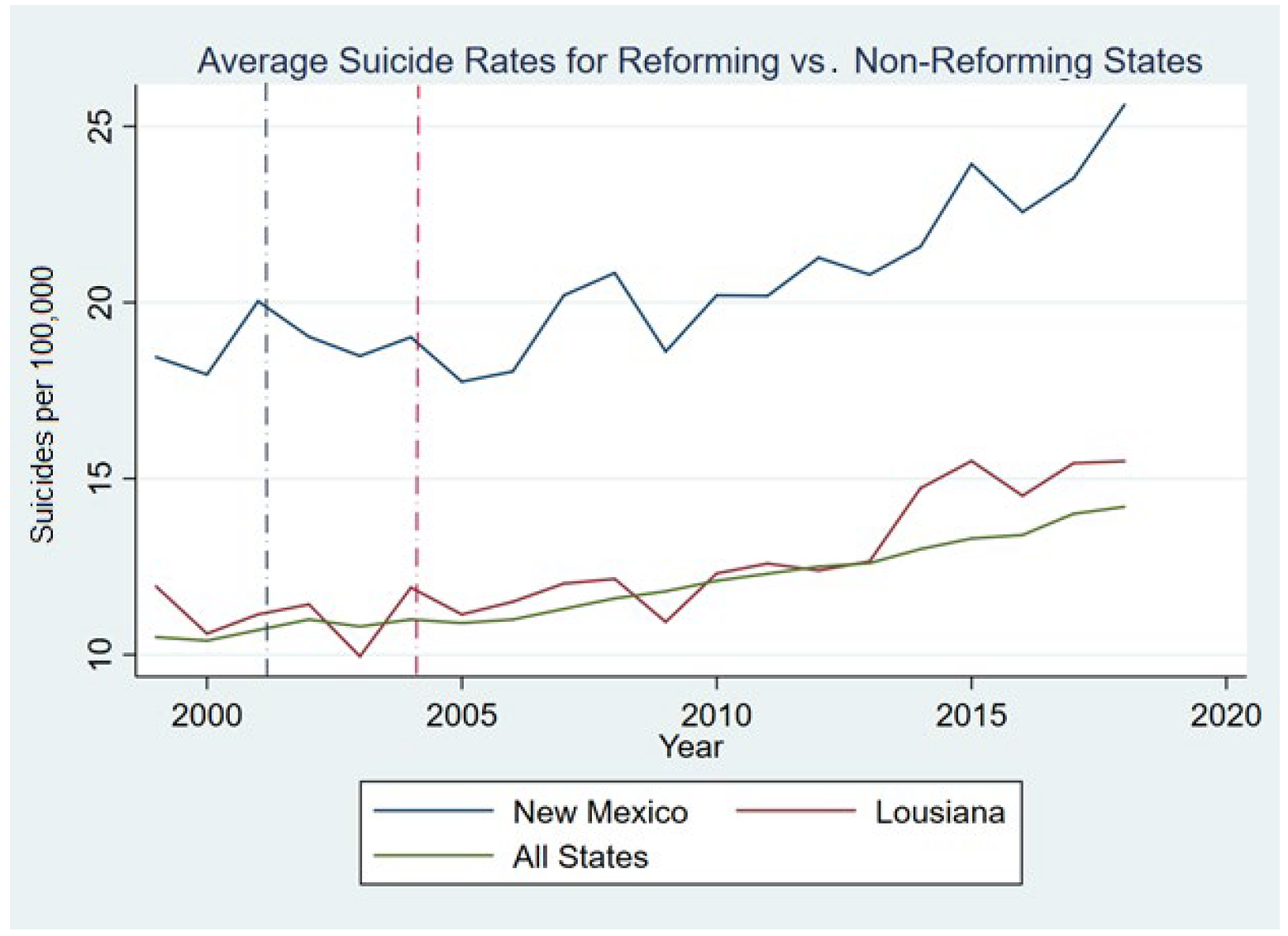
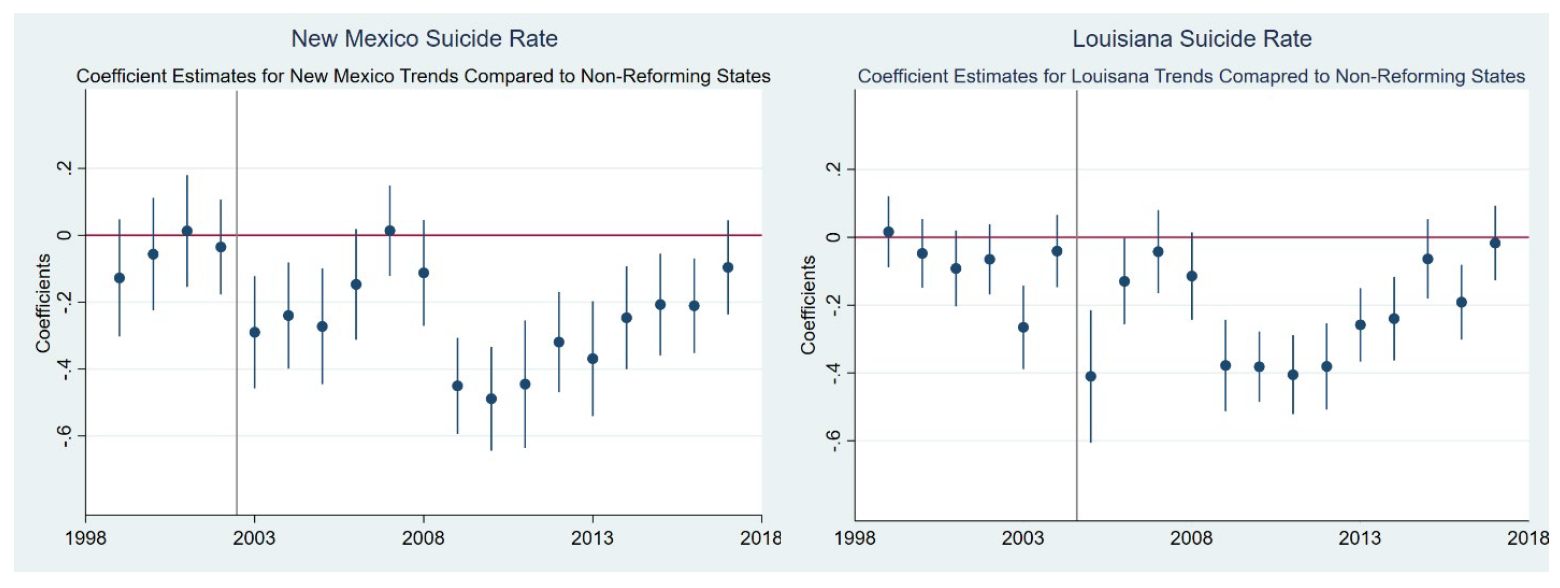
Figure 1 illustrates the average suicide rates per 100,000 individuals for New Mexico and Louisiana relative to the other states. Three things stand out when looking at this graph. First, we see that without controlling for any other factors that might affect suicide rates, New Mexico has a higher overall suicide rate compared to the other states, while Louisiana is more comparable to the national average. Second, the figure shows that the trends for the two reforming states are similar to the nonreforming states (which we include in our control group). Third, we observe that suicide rates have been increasing across all states between 1999 and 2018. We further graph the coefficients of the state-level suicide trend for New Mexico and Louisiana in Figure 2 and notice that our pre-policy change years are not significantly different from the national average trend in the pre-policy period.
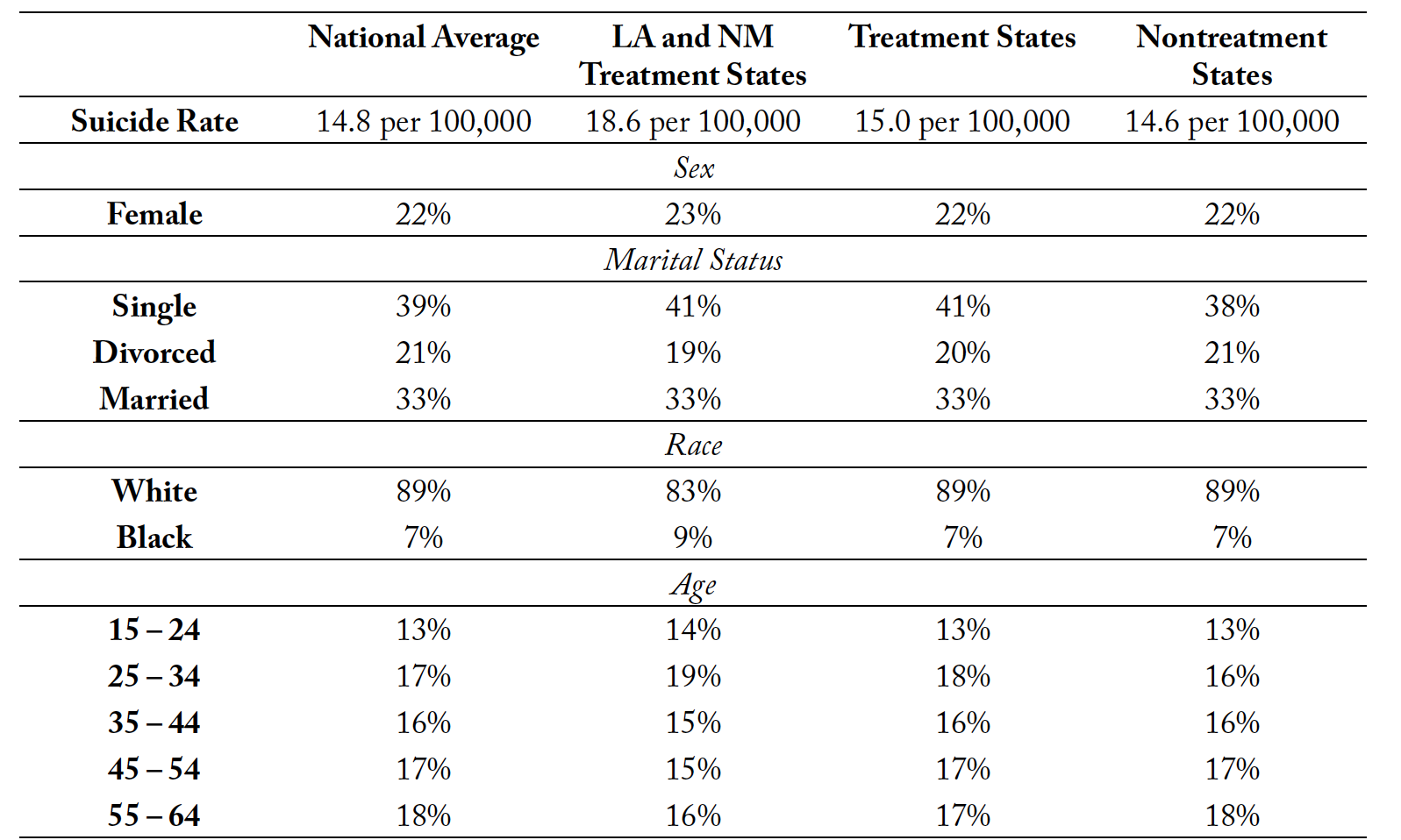
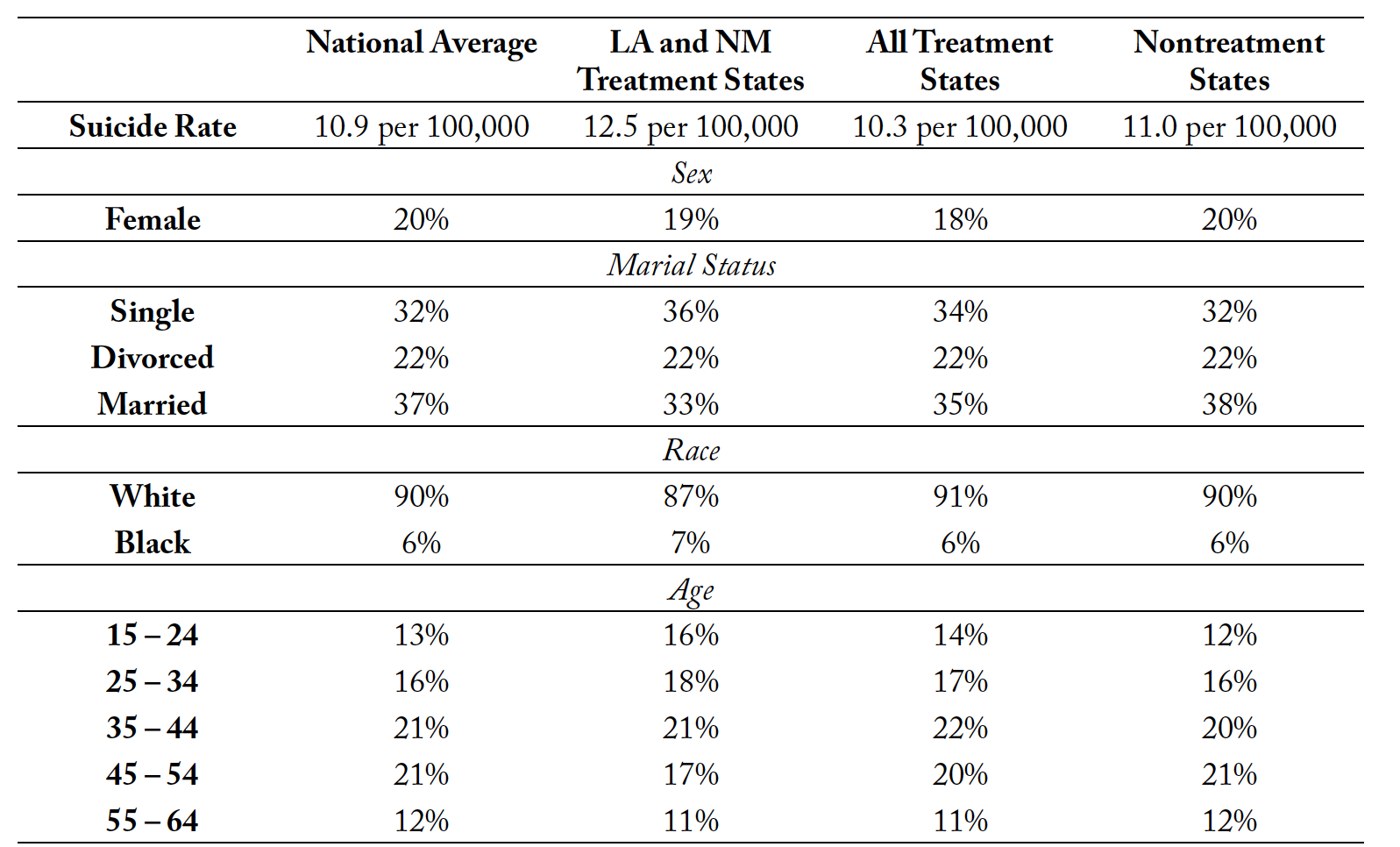
Tables 1 and 2 provides the summary statistics of some key variables that illustrate a snapshot of the mortality data, in the most recent sample year, 2018, and before any state changed their policies, 2003. Given the restrictions on data access, there are limitations in the data descriptions that we can report. We list the summary statistics of suicide rates for the nation, and then for the RxP states versus the nontreatment states, for years 2003 and 2018, the year before any policy changes and the last year in our sample, respectively. We see from the table that suicide rates increased from 2003 to 2018 for all groups. Suicide rates are also higher in the treatment states compared to the nontreatment states. This prompts the question of whether the policy implementation was endogenous or not, which we will discuss using a trend analysis. We also see that females only comprise a little over 20% of suicide deaths, which is consistent with the literature. Finally, according to our data, most of the suicides are of White individuals, which is also consistent with previous studies.
4. Methodology
We use a difference-in-difference estimation to investigate the impact of allowing psychologists to have prescriptive authority on access to mental healthcare and quality of care, as measured by suicide, the worst potential outcome. Our main specification is given below:
(1)
represents our outcome variables: natural log of suicide rates in a given month
in a state
in year
. We use suicide rates to detect how expanding prescription authority to psychologists affects quality of care.
is an indicator variable that equals 1 for states with prescriptive authority for psychologists, after the policy was implemented.
is 0 for all states that do not allow psychologists to prescribe controlled substances. Though five states have changed their scope-of-practice laws for psychologists, the only states that have had enough time since the policy change for the new training, education, and experience requirements to be implemented are New Mexico (since 2002) and Louisiana (since 2004).
Psychologists must complete certain training, education, and experience requirements before they are allowed to prescribe controlled substances. For instance, psychologists in New Mexico undergo 450 hours of didactic instruction and 400 hours of supervised practicum before they can prescribe (16 NM § 22.24). In Louisiana, psychologists must complete a postgraduate master’s degree in clinical psychopharmacology (About Prescribing Psychologists, 2014). Though the two states have differences in the way they describe their program, the legislation for prescriptive authority is very similar in terms of subject matter, timeline, practicum experience, collaboration requirements, and continuing education requirements. Since the policy was passed in different years for New Mexico and Louisiana, is 1 for New Mexico in 2003, 0 for Louisiana in 2003, 1 for both New Mexico and Louisiana in 2005 and later.
Our coefficient of interest is , which captures the impact of prescriptive authority.
and
represent state and time fixed effects, respectively. The control states contain all other 48 states. Since we are using staggered implementation periods, Louisiana is a control for New Mexico for 2 years. We assume that the changes in New Mexico policy are plausibly exogenous to Louisiana’s pre-reform suicide rate since the training and requirements for a psychologist to obtain prescriptive authority after the policy change in NM would take longer than the amount of time for LA to reform. We do not remove Illinois, Iowa, and Idaho from the control group since they have not had enough time since the policy change to fully implement changes.
Finally, to address for the differential timing of policy change between our treated states, we adopt the Goodman-Bacon (2018) decomposition to disentangle the impact of early adopters (New Mexico) from late adopters (Louisiana). Since both states implemented the law close to one another, we do not expect to see a vast change in the estimates. However, we might see an impact on the weights suggesting whether our estimates are driven mainly by New Mexico or Louisiana.
If expansion of scope of practice does not reduce the quality of mental healthcare, we would expect suicide rates to decline or remain unchanged. Studies within the occupational licensing literature have found mixed effects on quality of care metrics after scope-of-practice regulations were expanded for nurse practitioners. However, if access to mental healthcare improves, we would expect to see a significant decline in the rates of suicide. If the quality of healthcare diminishes, then we might observe an increase in mortality due to suicide. Therefore, the empirical result is theoretically ambiguous.
We further perform a series of subsample analysis to see whether the expansion of prescribing authority to psychologists had an impact on certain populations more than others. We expect larger impacts on minority groups due to greater access problems present in these communities. We also expect that the policy would have a bigger impact on people between the ages of 35 and 55. To test this, we conduct subsample analyses by the sex, marital status, age, and racial categories using the variables provided in the data set. Finally, all standard errors are clustered at the state level to adjust for unobservable confounders that are correlated to the treatment at the state level.
To account for potential confounding factors within states, we empirically go one step further and repeat our analysis with the addition of bootstrapped standard errors, with a rep of 100 and seed of 1. Boot- strapping is a computational method in which we empirically mimic the process of random sampling by treating our observed sample as if it were the population (Giné & Zinn, 1990). We then take samples of the pseudo-population, with replacements, and calculate our estimate of interest. This does not change the coefficient estimate itself but instead reevaluates the standard errors within the updated framework.
We check for parallel trends using Angrist and Pischke’s (2009) approach. We interact a linear time trend separately with each reforming state to account for the different timing of the policy change. The formal specification of this parallel assumption test is as follows:
(2)
The parallel assumption test is conducted separately for New Mexico and Louisiana and is applied to the
pre-reforming period. For New Mexico, is equal to 2002, representing the policy reform year, while for Louisiana,
is 2004. The main coefficient0 of interest is
, which captures the difference in trend between the reforming states and all the other states. When we conduct the specification for New Mexico, the control group includes all other states minus Louisiana. When we run the specification for Louisiana, we drop New Mexico from our analysis. We are interested in both the statistical significance and magnitude of
. If
is small in magnitude and statistically insignificant, we can argue that the parallel trend assumption is plausibly satisfied. X represents a vector of additional controls that are state and time specific, such as proportion of women who died of suicide, residential status, racial controls, education controls, marital status, and age, including macroeconomic variables such as unemployment rate. Finally, we also add a state-specific linear time trend
to capture the change in suicide rates over time within each state.
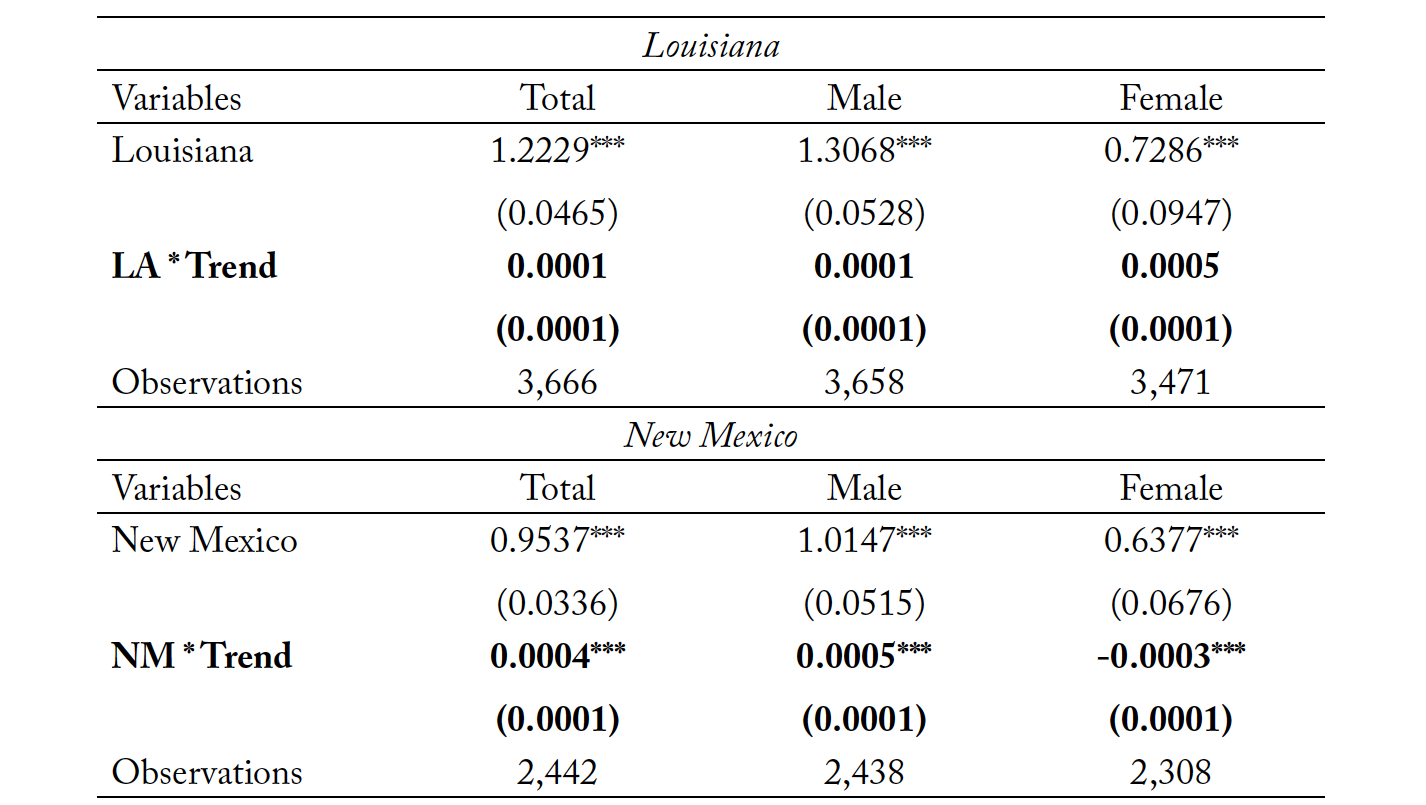
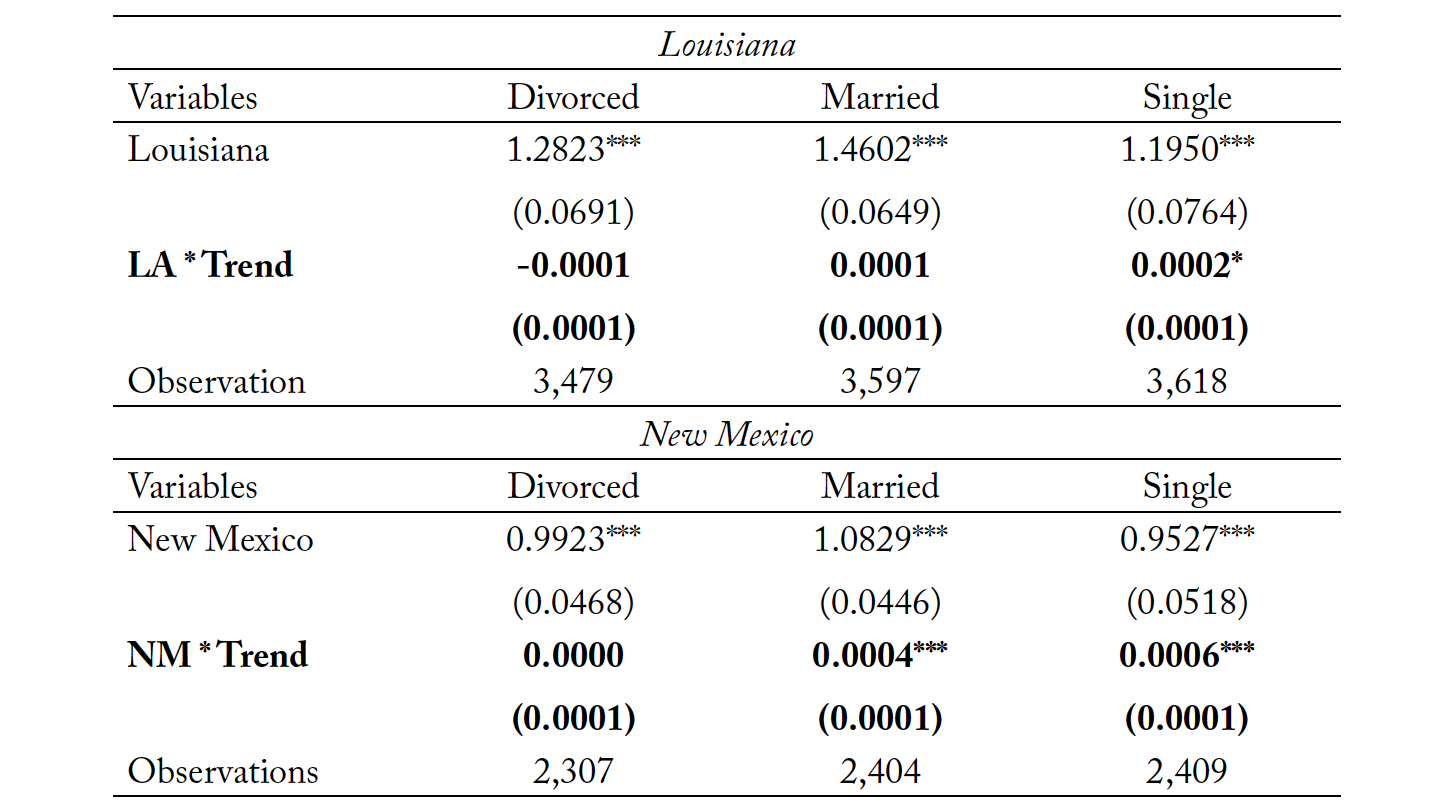
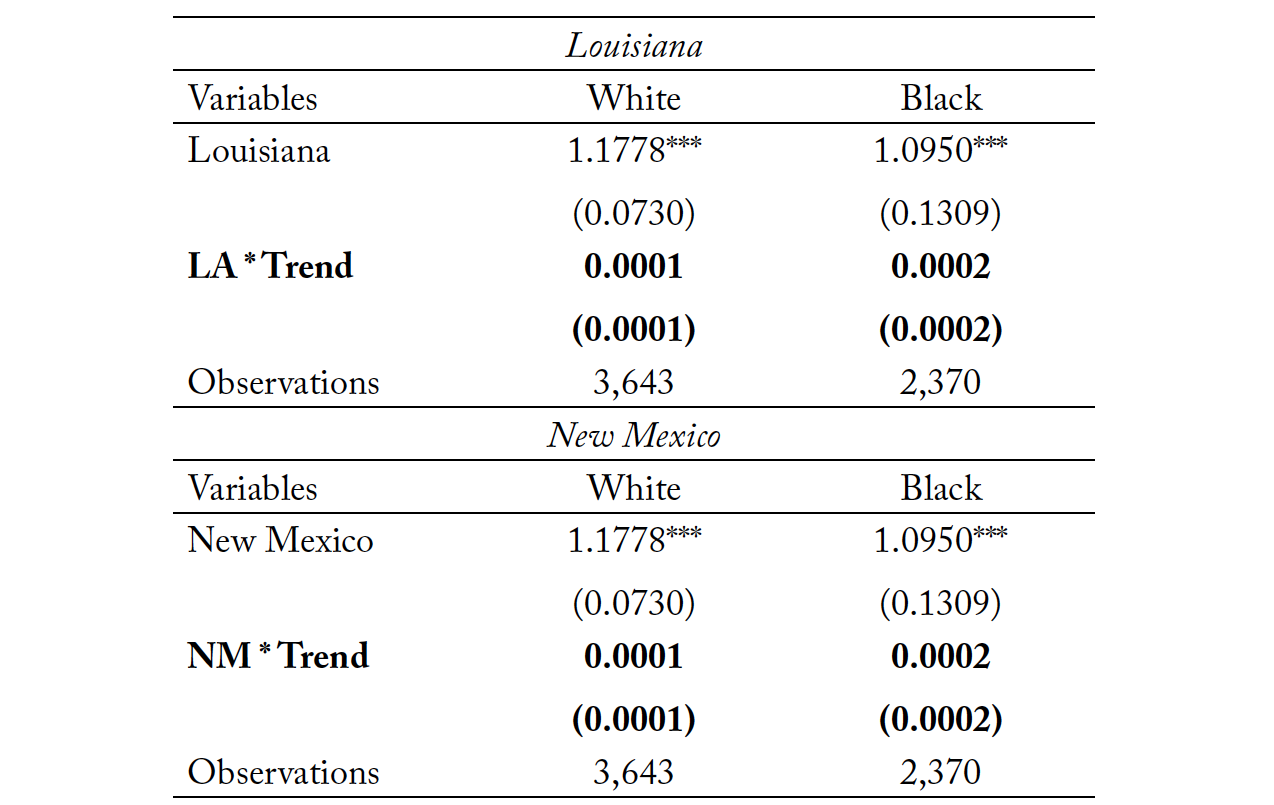
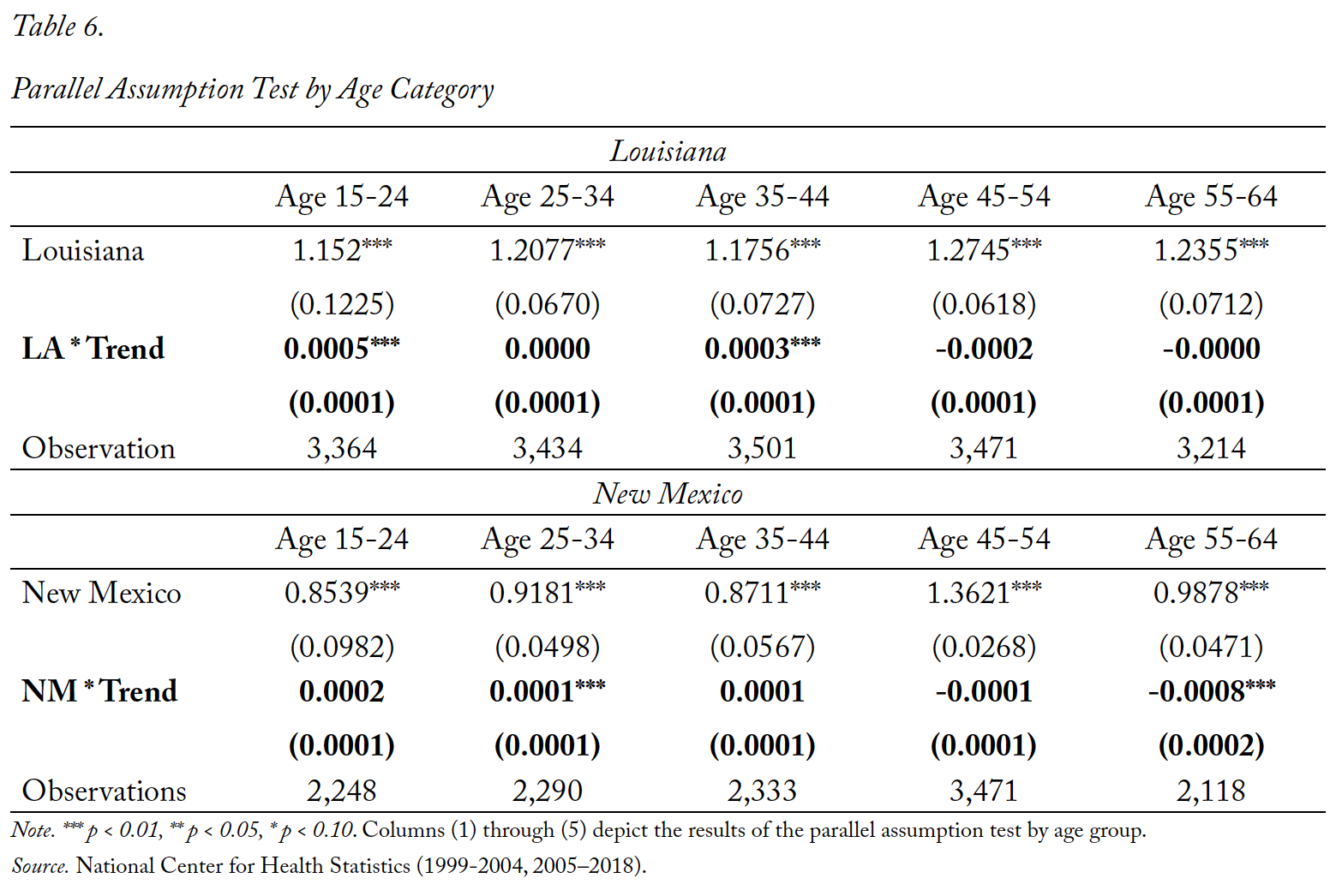
Though we inspect for pretreatment parallel trends using this methodology, it should also be understood that the parallel trends “test” is not a definitive test of common trends since the true counterfactual in which the states never changed their policy is unobserved. Regardless, inspection of pretreatment trends provides some comfort in the potential validity of parallel trends. We present the results of the parallel assumption test in Tables 3 through 6. Table 3 represents the trend analysis for New Mexico and Louisiana for the full sample, as well as both male and female subsamples. Tables 4, 5, and 6 repeat the analysis for marital status, race, and age, respectively. The coefficient of interest is both small in magnitude and statistically insignificant for most outcome variables. In the few cases where we find a statistically significant trend between reforming states and non-reforming states, the magnitudes are economically insignificant. The trend analysis also suggests that the pre-policy trend in suicide rates for Louisiana is statistically closer to the control group in the pre-policy period than New Mexico. However, the magnitudes of α for New Mexico are very small, when statistically significant.
5. Results
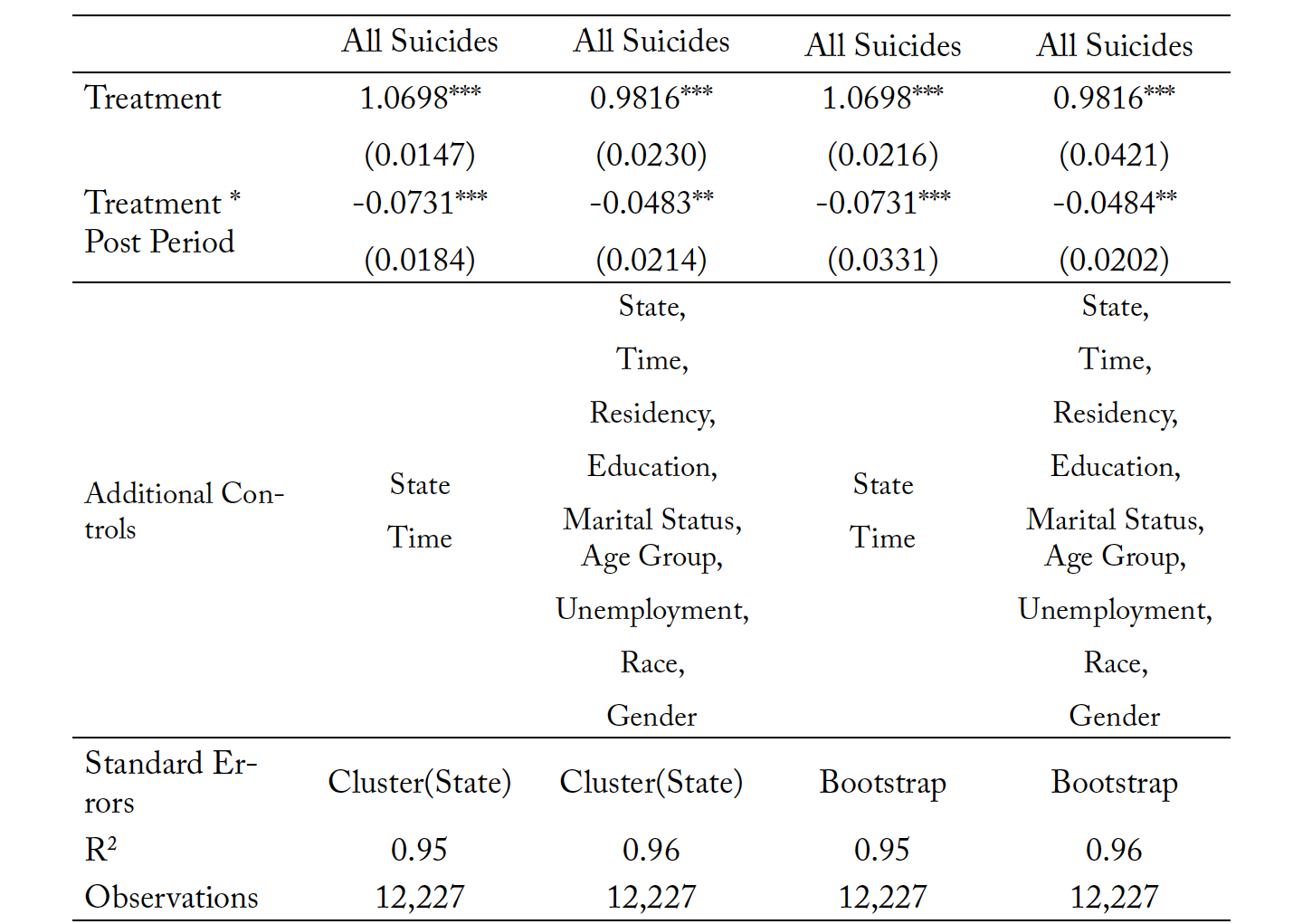
We present the regression results for the effect of prescriptive authority on logged overall suicide rates in Table 7. We find that overall suicide rates in our treatment states saw a reduction in the post-policy period of 5 to 7 percentage points, relative to states without prescriptive authority for psychologists. The most restrictive specifications contain controls such as state fixed effects, time fixed effects, and the proportion of suicides within that state for each residency status, education level, marital status, age group, race, and gender. The model also controls for state-level unemployment rates since lack of employment opportunities has been identified as correlated with suicide. These reductions are significant with standard errors clustered at the state level and with bootstrapped standard errors. The analysis is further conducted on a series of subsamples of mortality data by sex, marital status, age group, and race. Since the evidence suggests that access to mental healthcare services is underprovided for certain groups, we expect to see larger magnitudes of estimated changes in suicides for some groups relative to others.
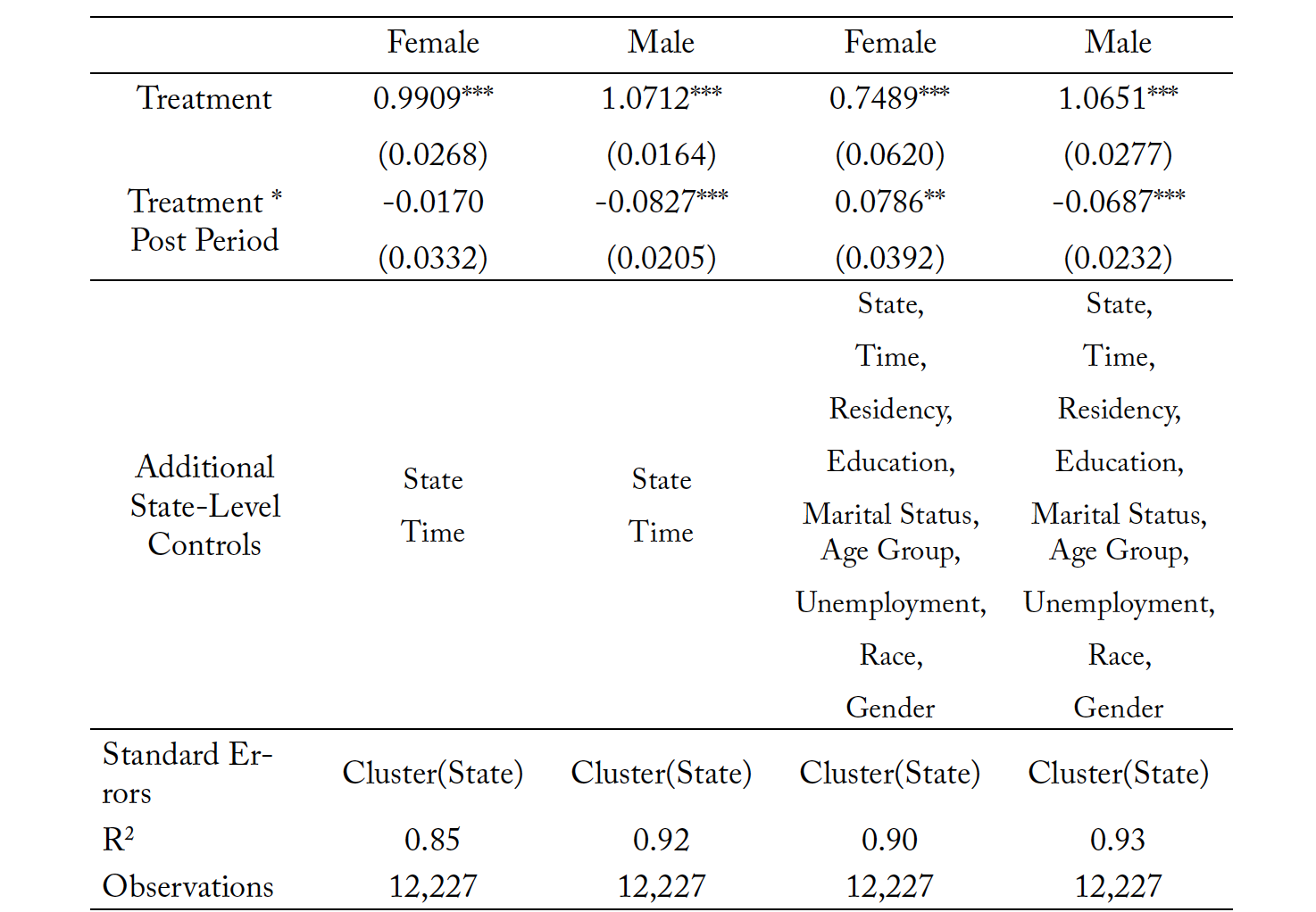
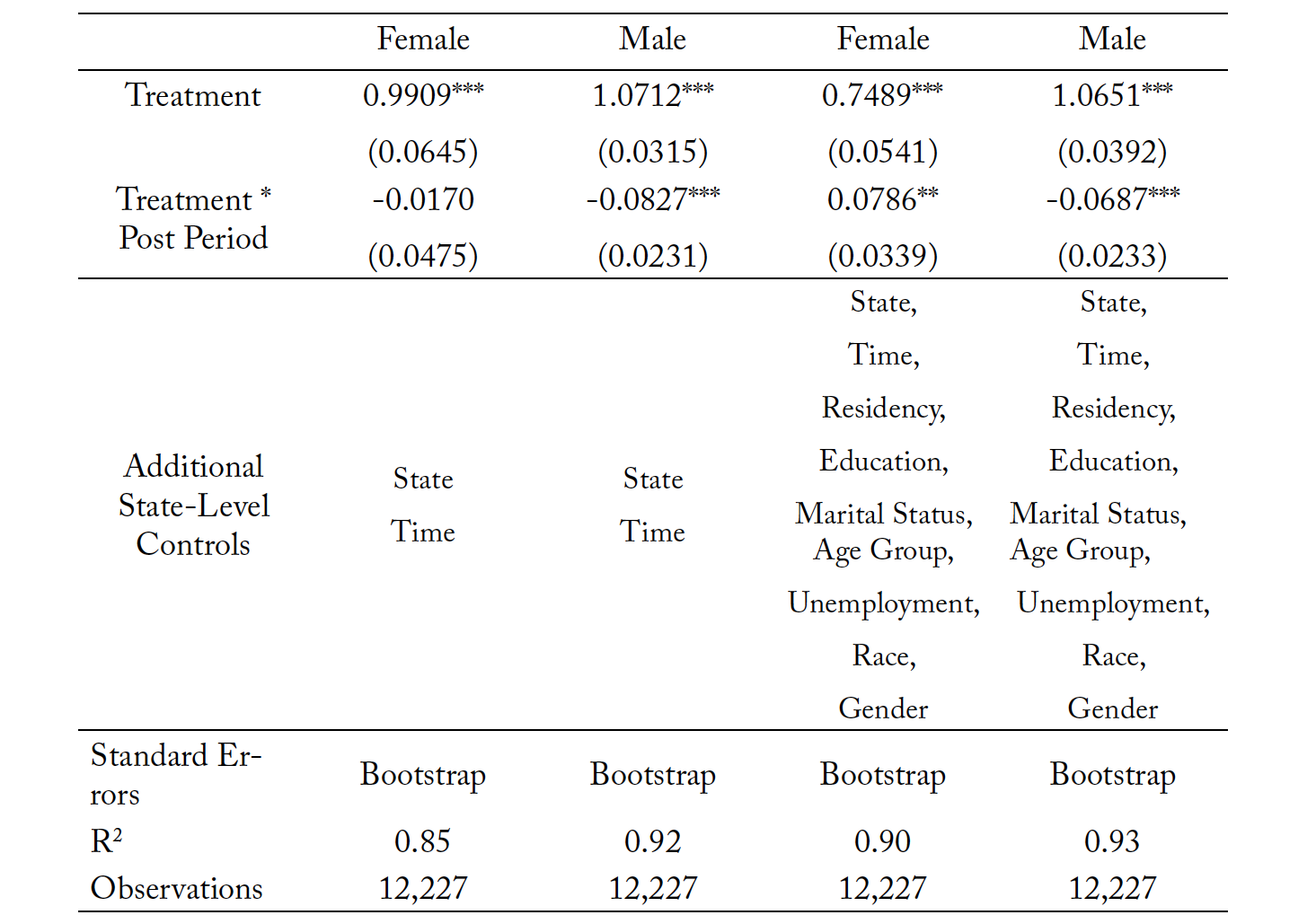
Table 8 shows that suicides decreased for males and increased for females in New Mexico and Louisiana following the passage of prescriptive policy for psychologists. This is interesting since male mortality due to suicide is higher, and females are a smaller sample of the suicide mortality population. The first two columns do not include additional controls. Our estimates suggest that the suicide rates for men in the reforming states decline by 7 to 8 percentage points. The coefficient for the female subsample is negative but statistically insignificant in the unrestricted model. However, in the restricted model, the female coefficient becomes significant and suggests that the mortality rates for females due to suicide increased by 8 percentage points. These results are counterintuitive and suggest that states should investigate qualitative data in their state on individuals seeking mental and behavioral health support to understand what their needs were before expanding prescriptive authority. Overall, suicides may decrease, but some subpopulations may be vulnerable to changes. Table 9 replicates these regressions with the addition of bootstrapped standard errors. In this case we find that there is still a significant increase in female suicide, but this significance is only at the 5% level. Males have a consistent significant reduction in suicide under the bootstrapped methodology.
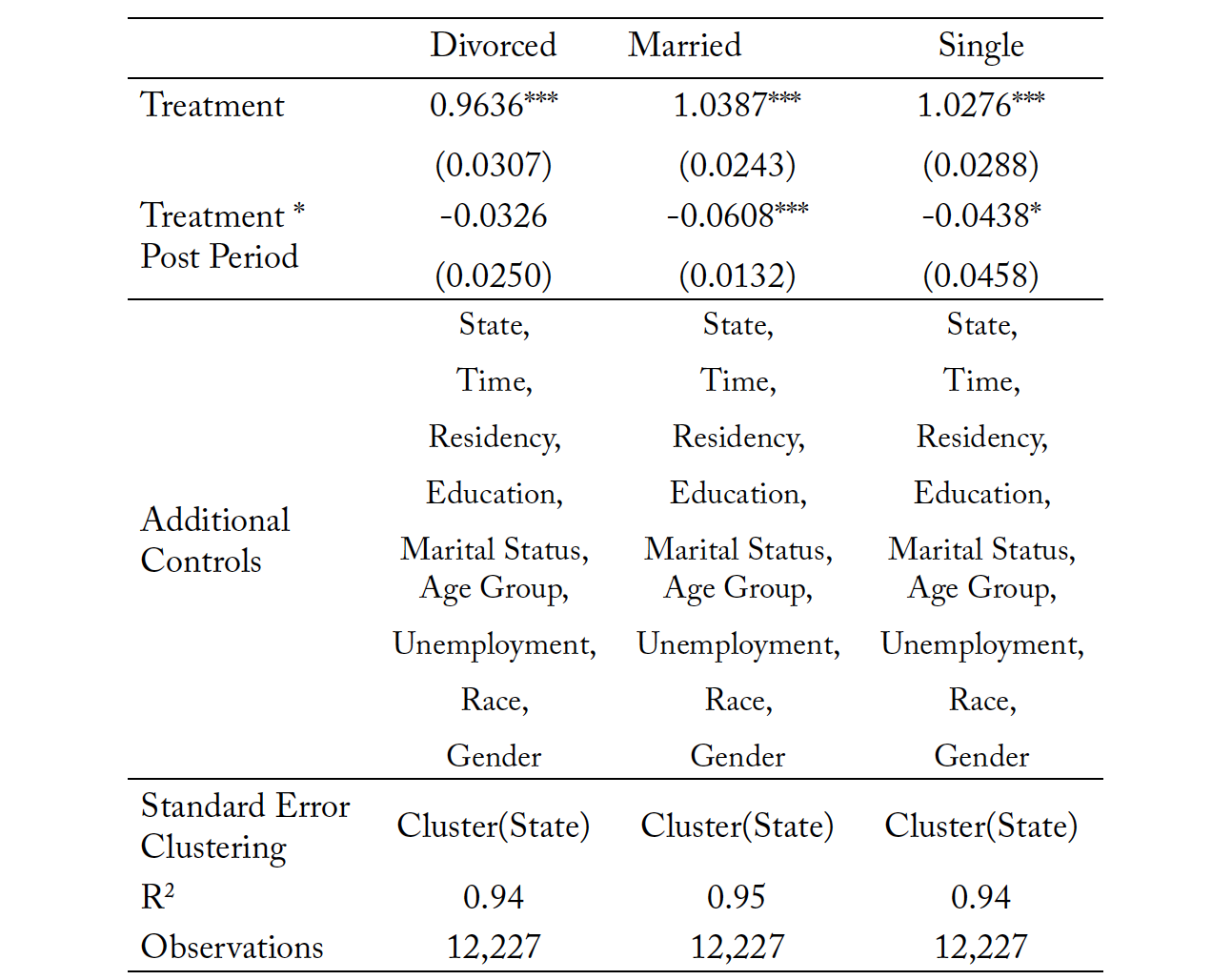
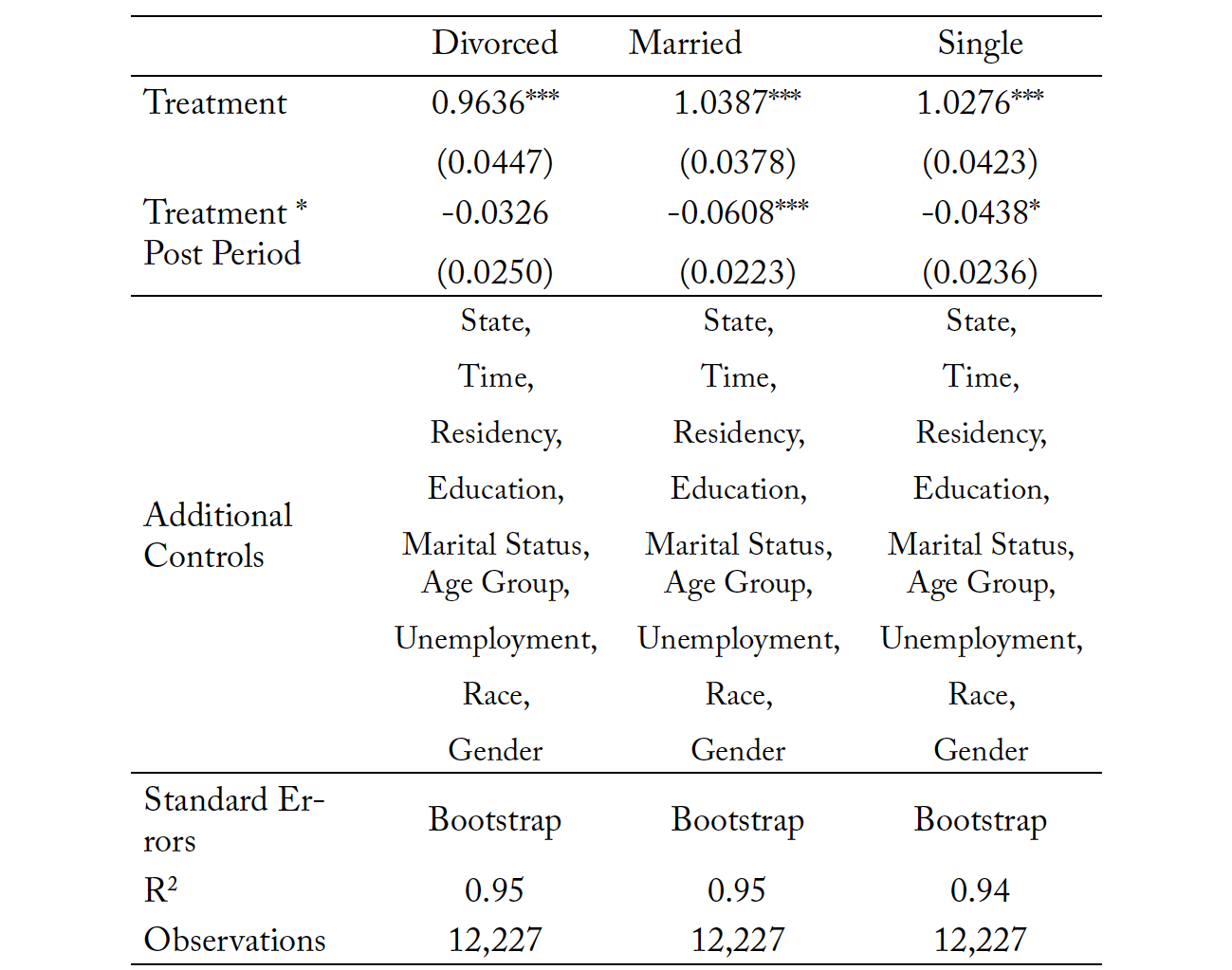
Tables 10 and 11 present the results for subsample analysis by marital status for both the clustered standard errors and bootstrapped standard errors, respectively. We see no statistically significant effect of the reform on divorced individuals, even though the point estimate is negative in magnitude. Suicide rates for single individuals and married individuals decline by 4 and 6 percentage points. The coefficient for single individuals is only significant at the 10% level. The direction and significance of results is consistent under bootstrapping. To the best of our knowledge, there has not been any study within the literature that looks at the prevalence of individuals with suicidal intentions in attending therapy with a psychologist or psychiatrist. Policymakers in each state should study their state’s suicide trends to determine the most at-risk category of people not receiving support. If there is substantial loss of life among married and single individuals, then expanding scope of practice for psychologists to prescribe pharmacological drugs may reduce suicide for these groups. If the concern is divorced individuals, then expanding scope of practice for prescriptive authority does not reduce suicide, but importantly, it also does not increase suicide. In other words, access could be improved without substantial reductions in quality as measured by the worst perceived potential outcome: the loss of life.
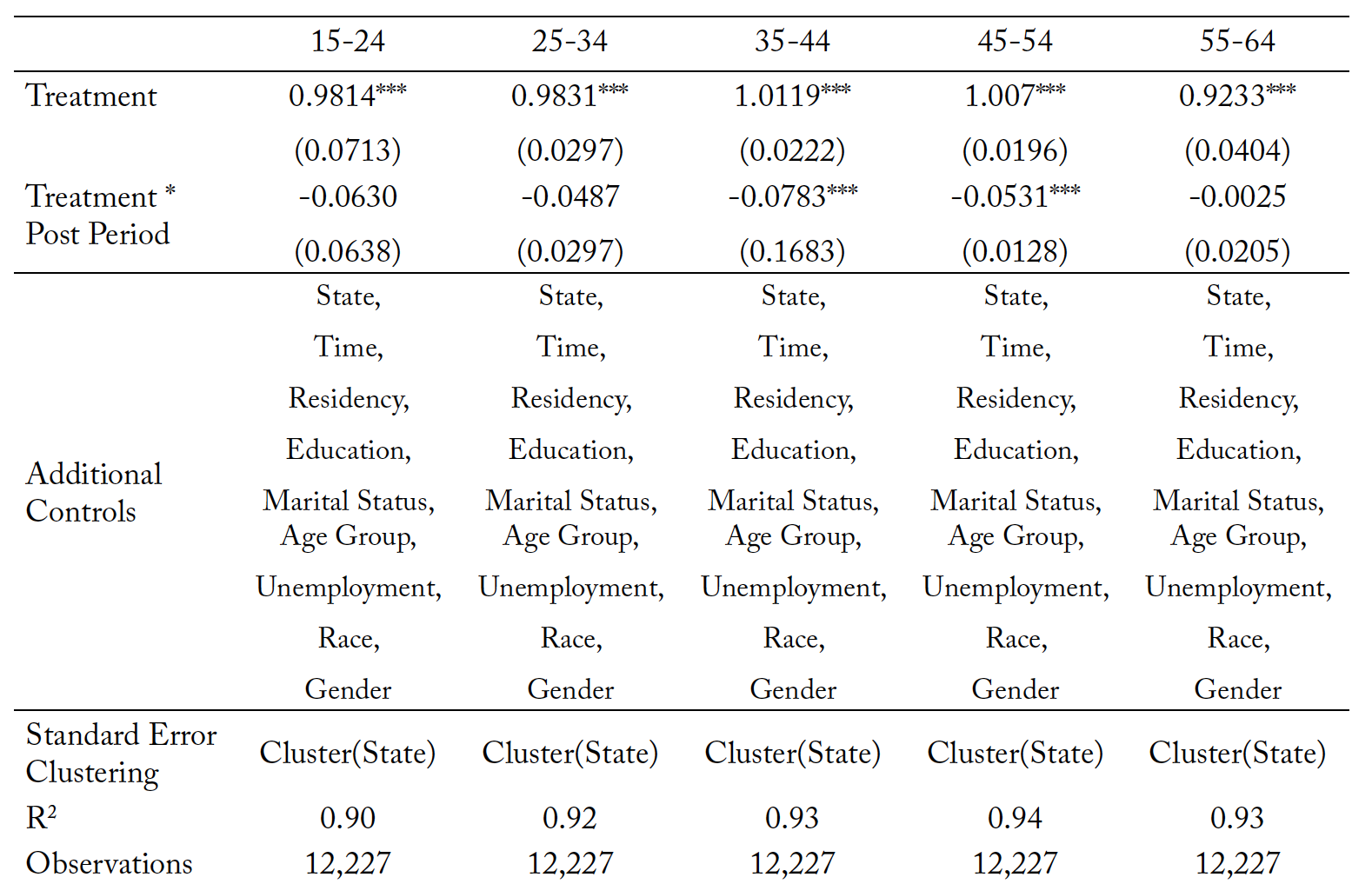
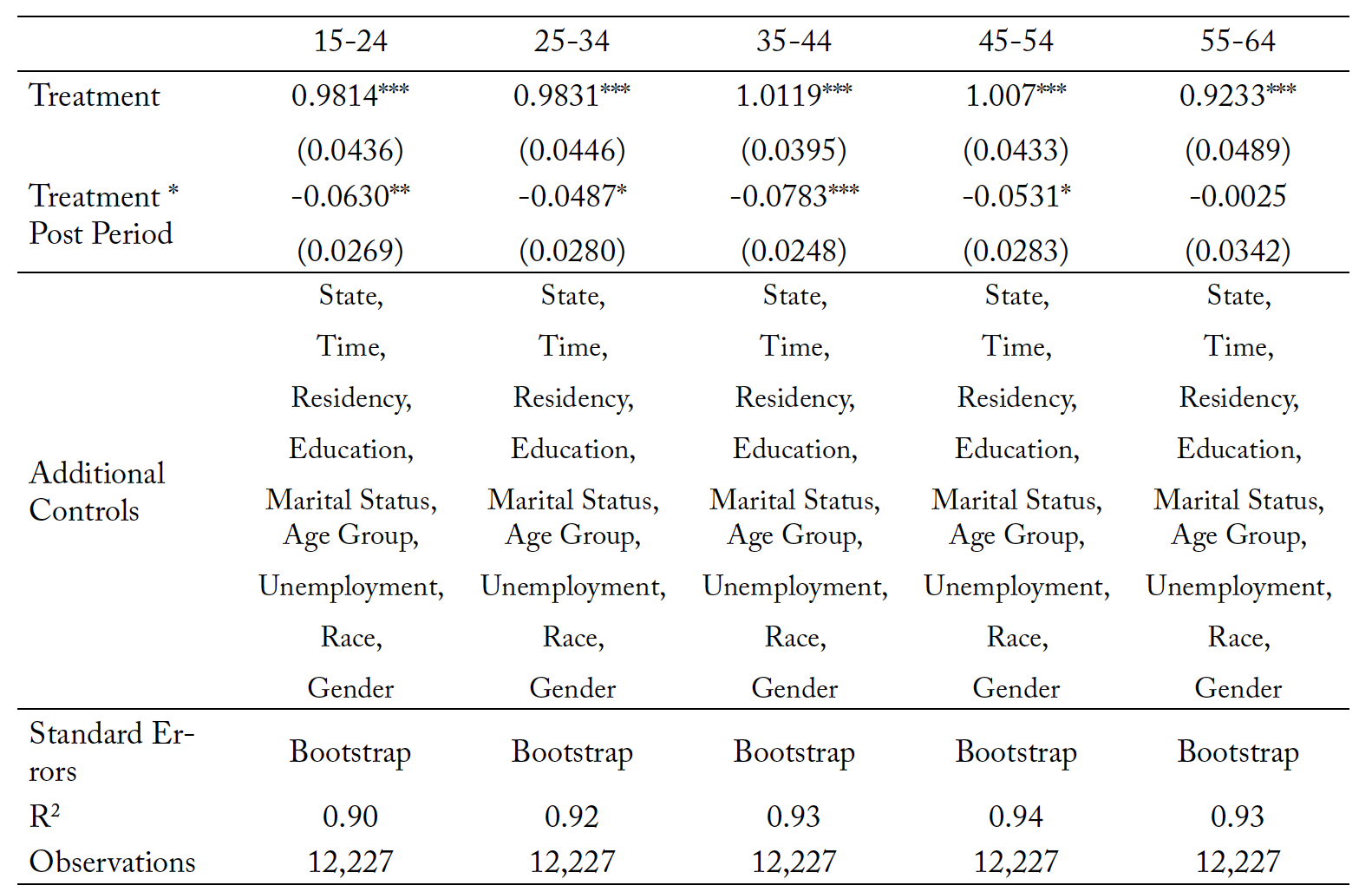
Table 12 presents results for different age categories. Table 13 repeats the analysis within the bootstrapped standard error framework. All the coefficients are negative in magnitude, but only significant for age groups 35–44 and 45–54 in the base model. Under bootstrapping we observe significance for ages 15–24, 25–34, 35–45, and 45–54. Reductions in suicide rates are between 4 and 8 percentage points depending on age category, with the largest effects being observed in the 35–44 age range. Within the literature, late 30 and early 40-year-olds make up a disproportionately high percentage of the suicide population, meaning that policy interventions targeting this group can improve outcomes for the most at-risk category.
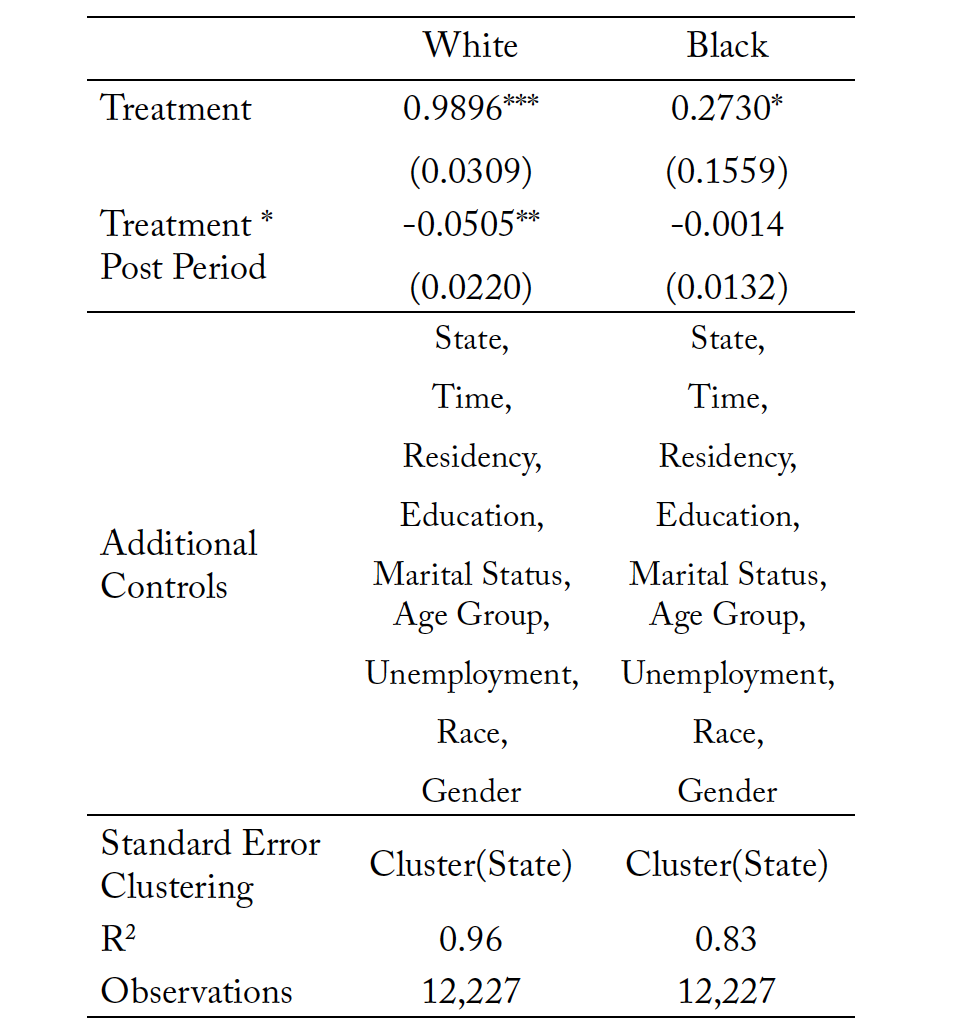
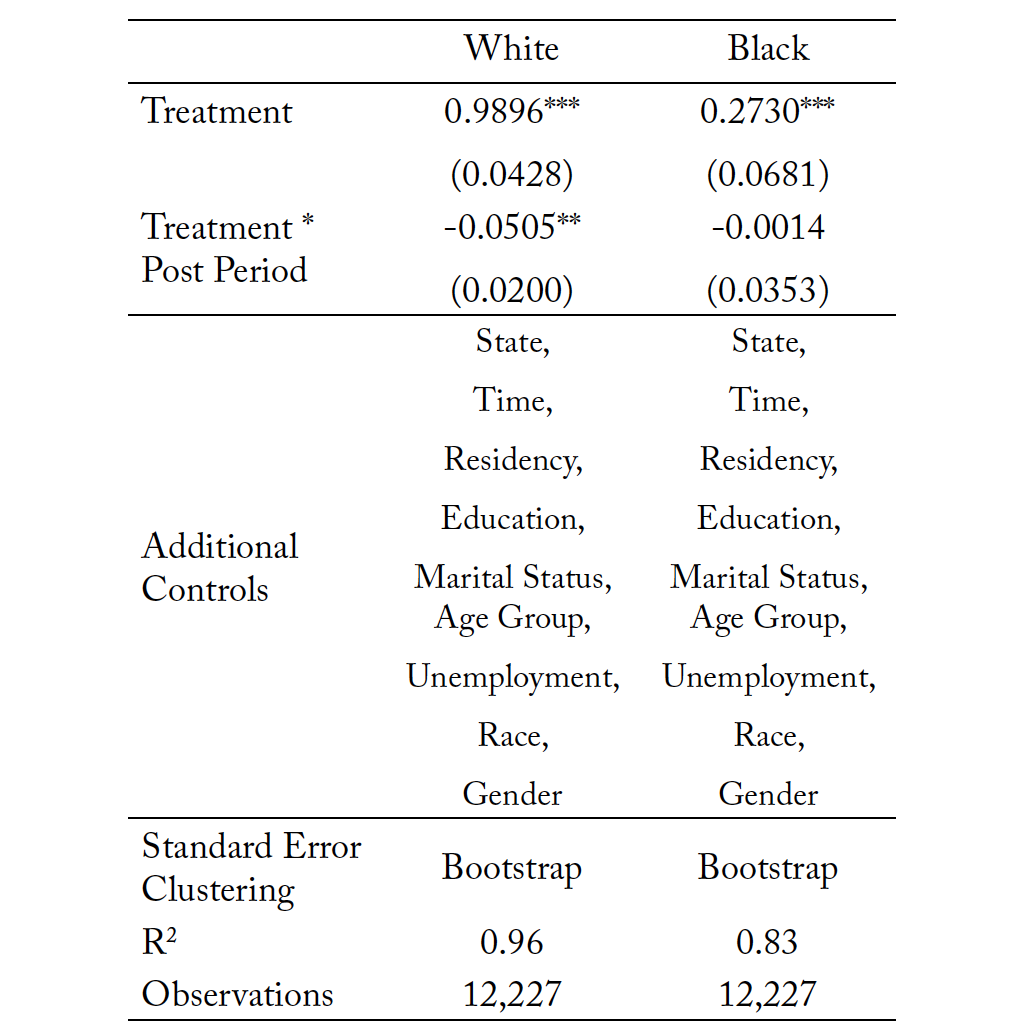
Finally, Tables 14 and 15 present the race subsample analysis with clustered standard errors and boot- strapped standard errors, respectively. Only the White coefficient is statistically significant at the 5% level within both model frameworks, suggesting a decline in deaths by suicide for White individuals by 5 percentage points relative to White individuals living in nonreforming states. There were no significant reductions in suicide within the Black community. Though there is not a reduction, there is also not a
significant increase. If the purpose of this prescriptive authority expansion is to improve access and address concerns about quality of care, a lack of increase is an intuitively interesting result. It means that access can be improved without worsening the most extreme mental and behavioral health outcomes.
We also conduct a variety of additional specifications, the results of which are presented in an online appendix that is available upon request. These additional tests include different forms of smoothing, such as a first order autoregressive model, exponential smoothing, and a random walk, and the results are nearly identical in magnitude and statistical significance.
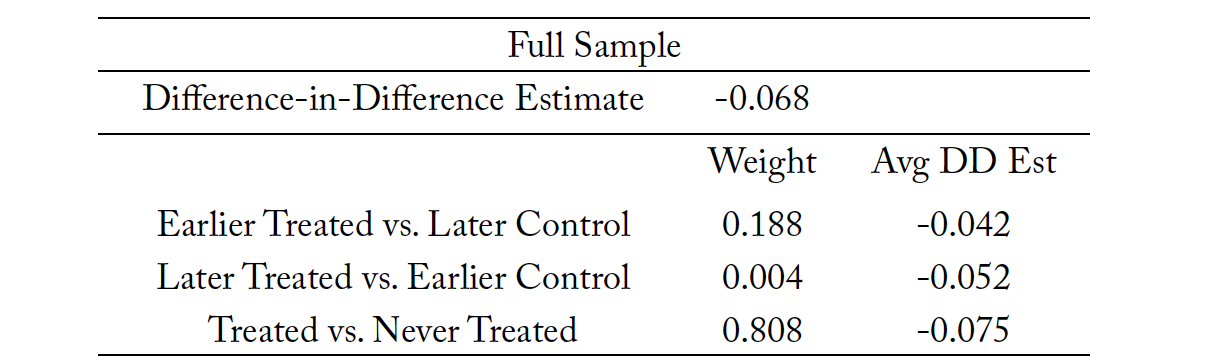
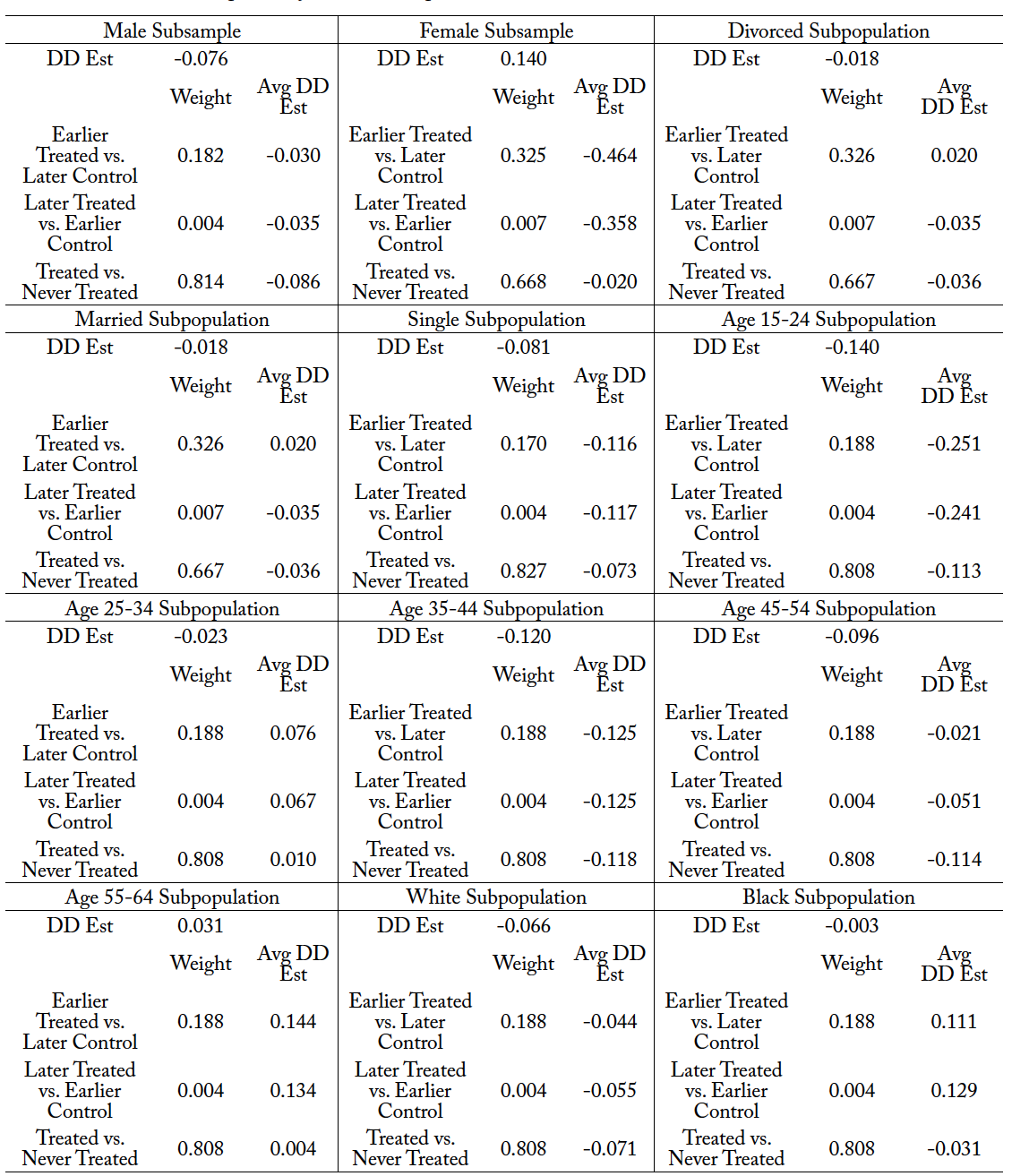
We conduct the Goodman-Bacon decomposition analysis for the full sample and several subsample analyses. The purpose of the Goodman-Bacon decomposition is to determine if the multiple treatment periods are biasing our difference-in-difference estimates. We present the results in Table 16 for the full sample. The results suggest that for the full sample, results are primarily being driven by the earlier treated groups rather than the later treated groups. The estimated difference-in-difference coefficient for the full sample suggests all three estimates are negative, suggesting that the mortality rate due to suicide is declining between all three treated groups versus the control group. However, the effects are largely being driven by the early treated units compared to the later treated units. We conduct this for all the groups in our analysis in Table 17, and none of the models cause the difference-in-difference estimator to be significantly different after accounting for early and late treatment periods.
6. Conclusion
Limited access to healthcare is linked to poorer health outcomes for many people. This is also true for mental healthcare. Economists and healthcare professionals argue that access to healthcare can be expanded by relaxing scope-of-practice regulations for providers. However, opponents of scope-of-practice expansions argue that the quality of care will be compromised, and the cost of care will increase due to overprescribing or overtesting. Our paper investigates how allowing prescriptive authority to psychologists affects suicide rates, which we argue is the most extreme of mental and behavioral health outcomes and one of the fundamental quality effects involved in prescriptive authority expansions.
Using a restricted mortality data set from the National Center for Health Statistics, we investigate the relationship between suicide and prescriptive authority for psychologists by employing a difference-in-difference estimation technique. In the United States, there can often be weeks or months between the time a psychologist identifies that a patient needs pharmacological intervention and when that patient is able to be seen, assessed, and given treatment by a separate psychiatrist (Malowney et al., 2015). Those weeks or months can be a matter of life or death for individuals with suicidal intentions, but expanding psychologists’ prescriptive authority reduces this time delay. Currently, five states have implemented prescriptive authority for psychologists, but it takes a few years for psychologists to fulfill all the requirements to obtain this privilege. Thus we limit our analysis to New Mexico and Louisiana, since they are the only two states to have had enough time for the policy to be integrated.
We find that states that have passed the prescriptive authority laws for psychologists have a 5 to 7 percentage points decrease in their overall suicide rates. These results are diverse within subgroups, with male, married, single, young, and White individuals seeing the largest reduction in suicide rates. We also find some evidence of an increase in female suicide and null results for divorced and Black subgroups. The United States is on the verge of a suicide crisis. Nearly every state has seen substantial increases in suicide rates over the past decade, and policy interventions that address access issues may be one of the most impactful ways to address this growing concern. Policymakers considering expanding the prescriptive authority of psychologists should first analyze trends within the subpopulations, as these expansions may be more impactful for some groups. Regardless, outside of the weakly significant effects for the female population, improving access to pharmacological intervention is not found to worsen the most extreme of quality measures, suicide.
Our results reflect trends that are similar to those observed by Alexander and Schnell (2019), who find that independent prescribing by nurse practitioners reduces suicide-related mortality. It should be noted that there are substantial differences between nurse practitioners and psychologists, and in insurance companies’ willingness to cover care. Alexander and Schnell (2019) did not find a reduction in mental health-related mortality when considering all counties, though they did find significant reductions (11%) in counties that are categorized as underserved. We are not able to present results at the county level due to our data usage agreement, but we do find significant reductions in suicide rates between 5 and 7% when considering the entire sample, unlike this previous work. Our results are intuitively similar, but direct comparisons between nurse practitioner and psychologist expansions are not able to be made at this time.
Our analysis is limited to one quality outcome measure, suicide, but it is certainly not reflective of all measure of quality outcomes. We suggest that future research investigate the relationship between these prescriptive authority expansions and a variety of other outcomes, such as depression, anxiety, cost of services, time to diagnosis, time to treatment plan, and the implications for wages for psychologists, psychiatrists, nurse practitioners, physicians, and professionals in other related medical fields.
Our paper suggests that allowing healthcare providers to prescribe controlled substances can improve access to mental and behavioral healthcare services. This is especially important for policymakers to consider now because the United States has been observing a shocking increase in suicide and has also been battling a global pandemic, which is likely to have long-lasting impacts on the population’s physical and mental health. Given recent CDC reports that suicide ideation has increased in young adults during COVID-19, we expect to see a rise in the demand for mental health services (Czeisler et al., 2020).
Restrictive scope-of-practice regulations reduce access to efficient mental healthcare, which is becoming a more prevalent concern as we emerge from the current pandemic. Our paper suggests that by allowing psychologists to prescribe psychotropic substances, there are reductions in suicide rates and increased access to sufficient treatment.
Appendix
Figure 1.
Figure 2.
Table 1. Summary Statistics for Suicide from the Vital Mortality Statistics Sample in 2018
Note: +/- 1.5% for rounding and missing data values. Summary statistics are provided for some select categories. Inclusion or exclusion of variables was determined by the limitations within the data usage agreement for the restricted Vital Mortality Statistics.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 2. Summary Statistics for Suicide within the Vital Mortality Statistics Sample in 2003
Note: +/- 1.5% for rounding and missing data values. Summary statistics are provided for some select categories. Inclusion or exclusion of variables was determined by the limitations within the data usage agreement for the restricted Vital Mortality Statistics.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 3. Parallel Assumption Test for Full Sample
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Column (1) analyzes the full sample of observations, while Columns (2) and (3) provide a subsample analysis of male and female observations, respectively.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 4. Parallel Assumption Test by Marital Status
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Column (1) inspects the trend for the divorced subset populations, Column (2) repeats the methodology for the married subpopulation, and Column (3) repeats the analysis for the single subpopulation.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 5. Parallel Assumption Test by Race
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Column (1) depicts the results of the parallel assumption test for the White subpopulation, while Column (2) depicts the results of the parallel assumption test for the Black subpopulation.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 6. Parallel Assumption Test by Age Category
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Columns (1) through (5) depict the results of the parallel assumption test by age group.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 7. Mortality Due to Suicide: Full Sample
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Columns (1) and (2) use all five treatment states, while Columns (3) and (4) only use LA and NM. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 8. Mortality Due to Suicides: Subsample Analysis by Sex
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Columns (1) and (3) looks at female mortality due to suicide, while Columns (2) and (4) look at male mortality due to suicide. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 9. Mortality Due to Suicides: Subsample Analysis by Sex with Bootstrapped Standard Errors
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. Columns (1) and (3) looks at female mortality due to suicide, while Columns (2) and (4) look at male mortality due to suicide. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 10. Mortality Due to Suicides: Subsample Analysis by Marital Status
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 11. Mortality Due to Suicides: Subsample Analysis by Marital Status with Bootstrapped Standard Errors
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 12. Mortality Due to Suicides: Subsample Analysis by Age Group
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 13. Mortality Due to Suicides: Subsample Analysis by Age Group with Bootstrapped Standard Errors
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 14. Mortality Due to Suicides: Subsample Analysis by Race
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 15. Mortality Due to Suicides: Subsample Analysis by Race with Bootstrapped Standard Errors
Note: *** p < 0.01, ** p < 0.05, * p < 0.10. The treatment variable is the natural log of mortality resulting from suicide within each individual state, in each individual time period. Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 16. Goodman-Bacon Decomposition for the Full Sample
Note: Early T refers to early treatment states (New Mexico). Late T refers to Louisiana. Never treated refers to states that did not reform their scope-of-practice law allowing psychologists to prescribe controlled substances. The weights suggest which group contributes to the DD estimate.
Source: National Center for Health Statistics (1999-2004, 2005–2018).
Table 17. Goodman-Bacon Decomposition for All Subsamples
Note: Early T refers to early treatment states (New Mexico). Late T refers to Louisiana. Never treated refers to states that did not reform their scope-of-practice law allowing psychologists to prescribe controlled substances. The weights suggest which group contributes to the DD estimate. Source: National Center for Health Statistics (1999-2004, 2005–2018).
References
American Association of Nurse Practitioners. (2016). AANP national nurse practitioner sample survey. https://www.aanp.org/advocacy/state/state-practice-environment/state-policy-fact-sheets/new-mexico-state-policy-fact-sheet.
Alexander, D., & Schnell, M. (2019). Just what the nurse practitioner ordered: Independent prescriptive authority and population mental health. Journal of Health Economics, 66, 145–162.
Angrist, J. D., & Pischke, J. (2009). Mostly harmless econometrics: An empiricists companion. Princeton University Press.
Arsenault-Lapierre, G., Kim, C., & Turecki, G. (2004). Psychiatric diagnoses in 3,275 suicides: A meta-analysis. BMC Psychiatry, 4, 37.
Bachmann, S. (2018). Epidemiology of suicide and the psychiatric perspective. International Journal of Environmental Research and Public Health, 15(7), 1425.
Bishop, T., Press, M., Keyhani, S., & Pincus, H. (2014). Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry, 71(2), 176–181.
Brådvik, L. (2018). Suicide risk and mental disorders. International Journal of Environmental Research and Public Health, 15(9), 2028.
Bureau of Health Workforce. (2016). Designated health professional shortage area statistics. U.S. Department of Health and Human Services.
Centers for Disease Control and Prevention. (2018, June). CDC Vital Signs [Fact sheet]. https://www.cdc.gov/vitalsigns/pdf/vs-0618-suicide-H.pdf.
Chen, J., Meyerhoefer, C. D., & Timmons, E. J. (2020). The effects of dental hygienist scope of practice and autonomy on dental care utilization [Working paper]. Center for Growth and Opportunity at Utah State University. https://www.thecgo.org/research/the-effects-of-dental-hygienist-autono-my-on-dental-care-utilization/.
Chesney, E., Goodwin, G., & Fazel, S. (2014). Risk of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry, 13(2), 153–160.
Czeisler, M., Lane, R., Petrosky, E., Wiley, J., Christensen, A., Njai, R., Weaver, M., Robbins, R., Facer-Childs, E., Barger, L., Czeisler, C., Howard, M., & Rajaratnam, S. (2020, August 14). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.htm.
Dueker, M., Jacox, A., Kalist, D., & Spurr, S. (2005). The practice boundaries of advanced practice nurses: An economic and legal analysis. Journal of Regulatory Economics, 27(3), 309–329.
Federal Trade Commission. (2014). Competition and the regulation of advanced practice nurses.
Gibbons, R. D., Hur, K., Bhaumik, K. K., & Mann, J. J. (2005). The relationship between antidepressant medication use and rate of suicide. JAMA Psychiatry, 62(2), 165–172.
Giné, E., & Zinn, J. (1990). Bootstrapping general empirical measures. The Annals of Probability, 18(2), 851–869.
Goodman-Bacon, A. (2018). Difference-in-differences with variation in treatment timing [Working paper]. National Bureau of Economic Research. Doi:10.3386/w25018
Hartley, D., Hart, V., Hanrahan, N., & Loux, S. (2004). Are advanced practice psychiatric nurses a solution to rural mental health workforce shortage? [Working paper]. Maine Rural Health Research Center.
Health Resources & Services Administration. (2021, July 18). Health professional shortage areas (HPSA). Retrieved December 19, 2020, from https://data.hrsa.gov/topics/health-workforce/shortage-areas.
Hughes D., Jiang, M., & Duszak, R. Jr. (2015). A comparison of diagnostic imaging ordering patterns be- tween advanced practice clinicians and primary care physicians following office-based evaluation and management visits. JAMA Internal Medicine, 175(1), 101–107.
Kandrack, R., Barnes, H., & Martsolf, G. (2019). Nurse practitioner scope of practice regulations and nurse practitioner supply. Medical Care Research and Review.
Kleiner, M., Marier, A., Park, K., & Wing, C. (2016). Relaxing occupational licensing requirements: Ana- lyzing wages and prices for a medical service. The Journal of Law and Economics, 59(2), 261–291.
Kleiner, M., & Park, K. (2010). Battles among licensed occupations: Analyzing government regulations on labor market outcomes for dentists and hygienists [Working paper]. National Bureau of Economic Research. http://www.nber.org/papers/w165160.
Lang, M. (2013). The impact of mental health insurance laws on state suicide rates. Health Economics, 22, 73–88.
Langelier, M., Continelli, T., Moore, J., Baker, B., & Surdu, S. (2016). Expanded scopes of practice for dental hygienists associated with improved oral health outcomes for adults. Health Affairs, 35(12), 2207–2215.
Malowney, M., Keltz, S., Fischer, D., Boyd, J. (2015). Availability of outpatient care from psychiatrists: a simulated-patient study in three U.S. cities. Psychiatric Services, 66(1), 94–96.
McCarthy, J., Blow, F., Ignacio, R., Ilgen, M., Austin, K., Valenstein, M. (2012). Suicide among patients in the veterans affairs health system: rural-urban differences in rates, risks, and methods. American Journal of Public Health, 102(Suppl 1), S111–S117.
McMichael, B. (2017). The demand for healthcare regulation: The effect of political spending on occupational licensing laws. Southern Economic Journal, 84(1), 297–316.
National Center for Health Statistics. (1999–2004). Multiple cause of death data archive [Data set]. CDC WONDER, Vital Statistics Cooperative Program. https://wonder.cdc.gov/mcd-v2004.html.
National Center for Health Statistics. (2005–2018). [Vital mortality statistics][Data set]. Vital Statistics Cooperative Program.
Niederkrotenthaler, T., Logan, J., Karch, D., Crosby, A. (2014). Characteristics of U.S. suicide decedents in 2005-2010 who had received mental health treatment. Psychiatric Services, 65(3), 387–390.
Occupational and Professional Licensing Psychologists and Psychologists Associates Application Procedures: Two-Year Supervised Practice, Title 16 NM, § 22.24 (2009).
Olfson, M., Shaffer, D., Marcus, S. C., & Greenberg, T. (2003). Relationship between suicide antidepressant medication treatment and suicide in adolescents. JAMA Psychiatry, 60(10) 978–982.
Phillips, R. Jr., Bazemore, A., & Peterson, L. (2014). Effectiveness over efficiency: Understanding the primary care physician shortage. Med Care, 52(2), 97–98.
Slivinski, S. (2020). Members of the occupational licensing board and the barriers to entry [Research note]. Center for the Study of Economic Liberty. https://csel.asu.edu/research/publications/July-2020-research-note.
Stange, K. (2014). How does provider supply and regulation influence health care markets? Evidence from nurse practitioners and physician assistants. Journal of Health Economics, 33, 1–27.
Stein, J., Kapoor, K., Tootoo, J., Wagner, A., Andrews, C., & Miranda, M. (2017). Access to ophthalmologists in states where optometrists have expanded scope of practice. JAMA Ophthalmology, 136(1), 39–45.
Swan, M., Ferguson, S., Chang, A., Larson, E., & Smaldone, A. (2015). Quality of primary care by ad- vanced practice nurses: A systematic review. International Journal for Quality in Health Care, 27(5), 396–404.
Thomson Healthcare. (2007). Ranking America’s mental health: an analysis of depression across the states. Mental Health America.
Timmons, E. (2017). The effects of expanded nurse practitioner and physician assistant scope of practice on the cost of Medicaid patient care. Health Policy, 121(2), 189–196.
Timmons, E., & Norris, C. (2018). CLIA waiver pharmacy growth: How does broadening scope of practice affect the pharmacist labor market? [Working paper]. Mercatus Center at George Mason University. doi:10.2139/ssrn.3191398
Too, L., Spittal, M., Bugeja, L., Reifels, L., Betterworth, P., & Pirkis, J. (2019). The association between mental disorders and suicide: A systematic review and meta-analysis of record linkage studies. Journal of Affective Disorders, 259, 302–313.
Tondo, L., Albert, M., Baldessarini, R. (2006). Suicide rates in relation to health care access in the United States: and ecological study. Journal of Clinical Psychiatry, 67(4), 517–523.
Traczynski, J., & Udalova, V. (2018). Nurse practitioner independence, health care utilization, and health outcomes. Journal of Health Economics, 58, 90–109.
Xue, Y., Ye, Z., Brewer, C., & Spetz, J. (2016). Impact of state nurse practitioner scope-of-practice regula- tion on health care delivery: Systematic review. Nurse Outlook, 64, 71–85.



 U.S. News and World Report
U.S. News and World Report Health Policy
Health Policy