Introduction
With a rapidly growing population and an increasingly complex and risky health environment, the United States’ health care system is now challenged to sustain its capability to deliver health care services. The system’s most difficult impediment to addressing this challenge is the low availability of qualified health professionals. Its current and projected complements of primary care physicians pale in comparison to its growing clientele.
In resolving the supply problem, the industry can potentially tap into the services of nurse practitioners as alternative primary care service providers. However, the effectiveness of this strategy relies on the nature of prevailing state legislation affecting the scope of nurse practitioners’ practice and prescription authorities, and the required extent of physicians’ supervision and collaboration. Different states have enacted scope-of-practice (SOP) laws granting varying degrees of professional independence to nurse practitioners. SOPs range from the more lenient full SOPs (in which nurse practitioners have full independence and do not need physicians’ supervision and collaboration) to the more restrictive SOPs (in which nurse practitioners do not have independence and require physicians’ supervision and collaboration).
This study focuses on SOP laws and their impacts on nurse practitioners’ ability to fully employ their knowledge to better serve their patients. This research examines linkages between the nature of SOP regulations and several health care labor market outcomes that include their work-time allocation, employment setting, task preference, and educational enrichment decisions.
Motivations and Study Goals
Accelerated increases in medical expenditures in the United States reflect a great demand for more medical resources and health professionals. The National Center for Health Statistics reports a stark increase in U.S. national health expenditures from $1,369 billion in 2000 to $3,492 billion in 2017. That represents a staggering 155.9% growth. Following the launching of federal public health reforms such as the Medicaid expansion in 2014, and with the demographic reality of an aging U.S. population, the U.S. health care system confronts mounting pressures to expand its resources and capabilities to accommodate the needs of its population. These needs include greater health care access for many segments in the society through more infrastructure investments and the employment of more qualified medical care providers.
The current reality, however, contends with a limited pool of available physicians. Their numbers have grown sluggishly over the years. Given the expected surge in demand for medical attention, the number of available physicians will soon become incapable of adequately servicing its projected clientele. Petterson et al. (2012) point out that the U.S. may face a shortage of about 15,000 to 32,000 primary care physicians in the year 2025. If this prognosis is not addressed with timely and effective solutions, the country’s public health conditions may seriously deteriorate.
Many states have already taken initiatives to solve the imminent physician shortage issues with alternative qualified health care providers. Among these alternatives are nurse practitioners, a group of advanced practice health professionals that receive intensive and qualified medical training, and thus are deemed capable of providing primary care services. They have become the most promising candidates for expanding the U.S. health care system’s capability to serve a wider population, particularly those in rural or economically disadvantaged areas.
Previous studies confirm that nurse practitioners have indeed made significant contributions to the provision of medical care in the U.S. (Barnes et al. 2018; Sonenberg and Knepper 2017). Moreover, they are among the fastest-growing groups of health professionals in the country. So far there are 290,000 nurse practitioners in the U.S. (American Association of Nurse Practitioners 2020). Projections indicate that the total employment of advanced practice nurses, including nurse practitioners, will increase by about 45% from 2019 to 2026 (Bureau of Labor Statistics 2020). Given the expected slowdown in the growth of new primary care physicians, nurse practitioners could play a crucial role.
A number of studies provide evidence on the impact of the SOP laws on health outcomes, health care ac- cess and utilization, and health service quality (e.g., Traczynski and Udalova (2018), Neff et al. (2018), Alexander and Schnell (2019), McMichael et al. (2019), Spetz et al. (2013), and Smith-Gagen et al. (2019)). In these studies, the nurse practitioners’ contribution in the health care delivery system is regarded as an important mechanism in achieving positive outcomes in the parameters analyzed. However, in spite of such strong empirical contentions, many states still impose restrictive SOP regulations that require nurse practitioners to provide patient care services with supervision by or collaborative agreement with physicians (National Association of Clinical Nurse Specialists 2020). Such policies could lead to suboptimal allocation of health care resources as nurse practitioners are excluded from assuming alternative primary roles in addressing the health care needs of a growing and aging population.
In contrast to restrictive SOP laws, full SOP regulations grant practice and prescription authority to nurse practitioners and do not require supervision by or collaboration with physicians. Full SOP regulations
are potentially the most beneficial under current health care industry conditions, as they do the most to increase health provider capacity (Kurtzman et al. 2017; Xue et al. 2018). Under this model, the supply of nurse practitioners may increase in terms of labor availability and working time. Previous related studies mostly focus on the changes in the number of nurse practitioners, but very few explore the working-time adjustment effects of the several versions of SOP regulations. Stange (2014) emphasizes the importance of the latter effect, which he thinks will help illuminate more comprehensively the labor market outcomes of SOP interventions as well as their impacts on people’s health.
Moreover, focusing merely on the change in the number of nurse practitioners in the short run may prove to be inadequate in understanding SOP-related labor market consequences. That is because nursing is a profession with high entry standards and barriers, including occupational licensure, lengthy graduate education and training, and migration restrictions among health care workers. When faced with some regulatory constraint, a typical instantaneous response of nurse practitioners would be a reduction in their working times, instead of completely exiting the industry. A study by Kleiner et al. (2016) examines working time adjustments and finds a significant increase of 65–75 hours of working time per year in a certain state after a prescriptive authority expansion was implemented. However, they point out that the 2002–2009 American Community Survey dataset used in their paper does not really separately identify nurse practitioners; thus, the dataset is not ideal for producing reliable, strong arguments on nurse practitioners’ working time responses.
The present study employs a difference-in-differences model that uses the geographic and temporal variations in the adoption of full SOP laws across states in the U.S. Implemented as a quasi-natural experiment, the model explores the impact of full SOP regulations on nurse practitioners’ labor-market participation decisions, such as those involving working hours and wages. The rich information from the quadrennial National Sample Survey of Registered Nurses (NSSRN) from 1980 to 2008 provided by the Health Resources and Services Administration enables us to expand the investigation of labor supply adjustments beyond working time and wage levels to other aspects, such as changes in employment settings, tasks, migration across states, and advanced nurse program enrollment. This study aims at providing a comprehensive evaluation of nurse practitioners’ labor supply decisions related to SOP laws. This study’s findings can provide insight for policymakers in their decisions about how much practice and prescription autonomy to give to nurse practitioners.
This study’s findings offer some important and unique contributions in this field of research. First, full SOP laws increase the weekly working time allocation of nurse practitioners but the average share of time devoted for patient care does not increase. Instead, full SOP encourages nurse practitioners to reduce time spent in supervision and re-allocates such time more toward performing administrative tasks. As a result, nurse practitioners may have more time to manage and run a clinic and expand medical services. Second, full SOP brings no change in hourly wages, and those results are consistent across different specification tests. Third, heterogeneity analysis presents evidence showing that areas with larger health care needs (rural or with more elderly residents) experience a higher increase in working time allocation from nurse practitioners with full SOP. Fourth, this study does not find migratory responses of nurse practitioners across states (whereby nurses in states with restrictive SOP would consider migrating to states with full SOP) but finds movement among different employment settings. For instance, nurse practitioners are more likely to work in an ambulatory care agency under full SOP laws. This may affect the accessibility of nurse practitioners for different populations that use certain health services.
Finally, evidence shows that full SOP laws induce registered nurses, particularly those with higher skill levels, to enroll in advanced nursing programs (master’s or PhD) that would eventually translate to higher quality of care provided by these more highly educated nurses. By encouraging qualified registered nurses to become nurse practitioners, a less restrictive policy environment would not only further expand the health worker labor complement in the long run but also increase the productivity and efficiency of the health care work force. These positive consequences could alleviate the impending concerns about the supply of health care services. Meanwhile, such a policy environment could also lead to a more equitable and comprehensive delivery of important and essential services to those in need of medical attention.
Background and Conceptual Framework
Nurse practitioners’ importance and scope-of-practice laws
Nurse practitioners are playing a more and more important role in the U.S. health care market. Most nurse practitioners have graduate degrees such as master’s degrees and receive further professional training. Their clinical education goes beyond the requirement for obtaining licensure as registered nurses.
There is a substantial overlap in functions and responsibilities of nurse practitioners and primary care physicians. Nurse practitioners are trained and capable to handle a wide range of patient services, including management of blood pressure and diabetes conditions, treatment of acute injuries and illnesses, chronic problem control, drug and treatment prescription, laboratory test ordering, patient counseling, and disease prevention.
Nurse practitioners also share certain functions with physician assistants. However, physician assistants are usually generalists in family medicine while nurse practitioners specialize in one sub-area within family medicine. These specialization options include adult, geriatric, pediatric, and neonatal care. In addition, most physician assistants receive medical program training for only two years, which is shorter than the requirement for the advanced nursing program.
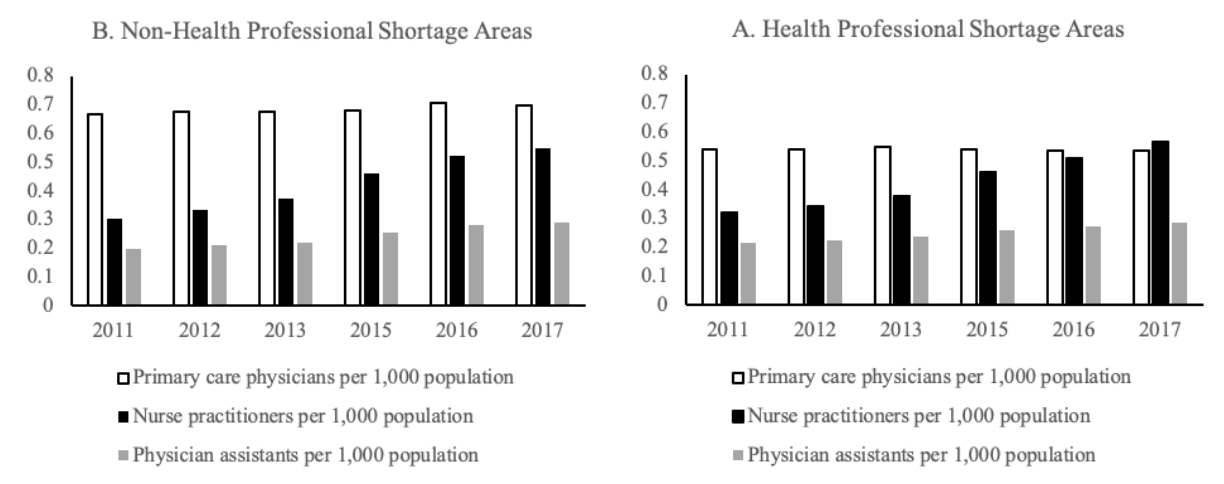
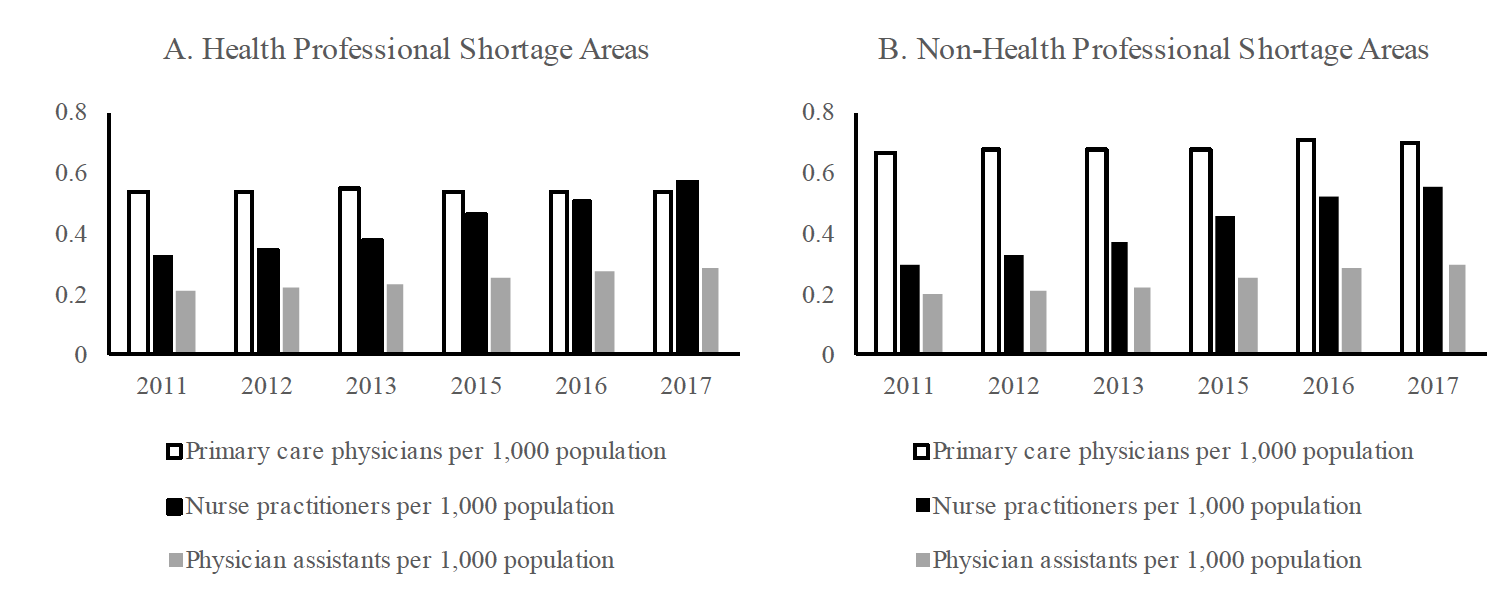
Despite the similarity in their health care service tasks, nurse practitioners differ from primary care physicians and physician assistants in their population growth and distribution in recent years. Figure 1 shows the number of primary care health professionals per 1,000 population in health professional shortage areas (HPSAs) and non-HPSAs.1The designation of HPSA status is provided by the Health Resources and Services Administration (HRSA). In general, HPSAs usually are rural regions with a high share of low-income residents and a predominantly farming population. As can be seen from plot A and plot B, HPSAs have lower numbers of health professionals. Among the three categories of primary care health professionals, nurse practitioners experienced the largest increase in their numbers in both HPSAs and non-HPSAs in recent years. In non-HPSAs, the number of nurse practitioners increased by 77% from 2011 to 2017 (from 0.31 to 0.55 per 1,000 population, respectively). The comparable growth rate for physician assistants is 45%, while primary care physicians had the lowest growth in these areas. The same trends are noted in HPSAs where nurse practitioners registered a 75% growth in the same period (from 0.32 to 0.56 per 1,000 population between year-end-points 2011 and 2017).
More importantly, nurse practitioners have overtaken primary care physicians in numbers in 2017, thus becoming the major health service providers in HPSA regions. As such, nurse practitioners have the strongest potential for closing the gap in providing medical care services. That gap will otherwise only widen as the number of primary care physicians continues to dwindle.
Figure 1. Trends in the number of health professionals per 1,000 population.
Source: The Area Health Resources Files — HRSA data
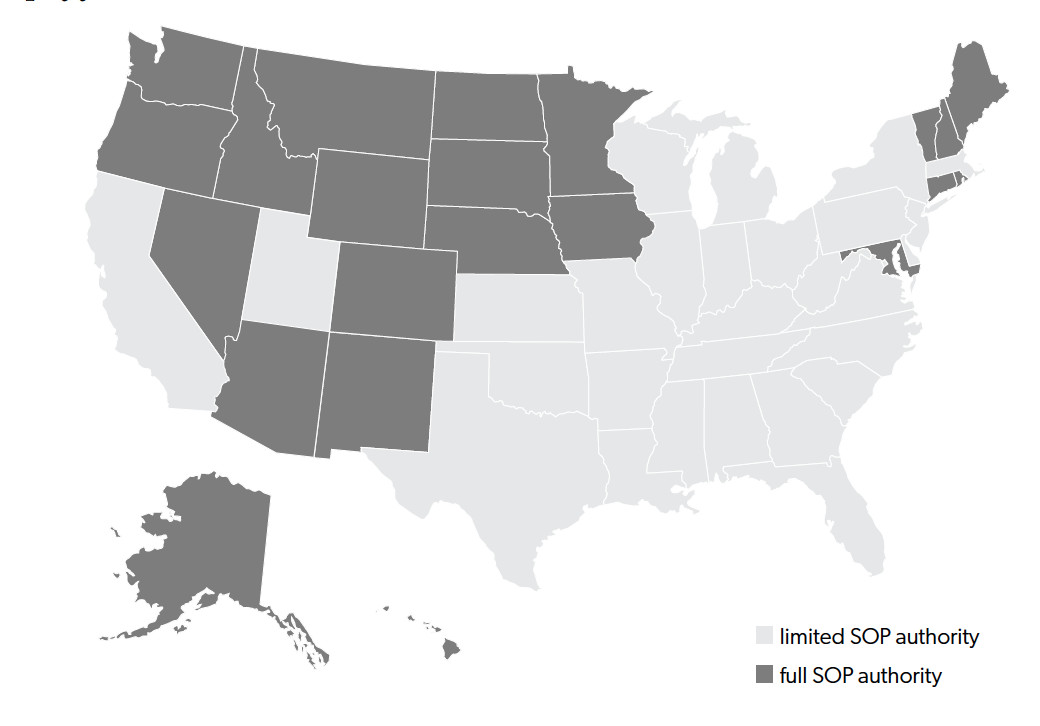
To take full advantage of the growing population of nurse practitioners, many states passed full SOP laws that granted full independence to nurse practitioners by allowing them total practice and prescription authorities, with no physician supervision or collaboration requirement. As the American Association of Nurse Practitioners (AANP) reports, in 2019 there were 22 states that had full SOP laws. This enables us to explore the impact of nurse practitioners’ occupational independence on their labor market outcomes using a difference-in-differences approach. A map of states that granted full SOP to nurse practitioners can be found in figure 2.
Figure 2. U.S. map of full and restrictive SOP laws
Source: The Annual Legislative Update from the Nurse Practitioner Journal 1984 to 2008.
Conceptual framework
A change in the regulatory environment from restrictive to nonrestrictive could lead to significant adjustments in the supply of and demand for nurse practitioners. On the supply side, a less restrictive practice environment may encourage nurse practitioners to increase their willingness to work by migrating from restrictive to nonrestrictive SOP state environments. They may also decide to increase their working time allocation. Moreover, a more relaxed SOP regulatory environment may encourage more registered nurses to become nurse practitioners by enrolling in advanced nursing practice programs.
Kleiner et al. (2016) and McMichael (2018) identify five mechanisms through which SOP restrictions may affect nurse practitioners’ labor supply decisions. First, in the presence of a physician supervision requirement, nurse practitioners may have limited opportunities to choose to work in remote and rural areas usually shunned by physicians. Second, besides remote and rural areas, there are also some other areas with a limited number of physicians; nurse practitioners also inevitably give up practicing in these areas where they cannot find supervisory physicians. Third, the extra administrative costs imposed on nurse practitioners by restrictive SOP laws may discourage them from providing more services. Fourth, restrictive SOP laws may put a downward pressure on the wages of nurse practitioners and discourage them from working more hours. Fifth, lacking in the occupational fulfillment brought about by gaining professional independence, nurse practitioners may not be as incentivized to provide more working hours as they could be under full SOP laws. Notably, Sass and Nichols (1996) point out that certain health professionals, such as physical therapists, were actually willing to pay the price of lower wages in return for some gains in being allowed professional independence.
On the demand side, expanded or full SOP laws may also induce people to alter their demands for nurse practitioners’ services. Stange (2014) contends that the noncompetitive structure of the primary care market would allow it to absorb quickly any increase in the labor supply of nurse practitioners. McMichael (2018) argues that nurse practitioners may “backfill” regions with health care delivery issues due to their inadequate pools of physicians. In these areas, the nurse practitioners’ services do not have any crowding-out effect on physician’s services. Markowitz et al. (2017) point out that the demand for nurse practitioners’ services may increase as more health care facilities are established. In addition, Timmons, Hockenberry, and Durrance (2016) and Markowitz et al. (2017) suggest that expanded SOP laws would alter the patients’ “taste” or perceptions of services provided by nurse practitioners and therefore would lead to increased demand. Moreover, expanded SOPs that make nurse practitioners more accessible to their clients would entice more people to seek medical help. In the absence of a more tolerant SOP law, these patients would have considered forgoing or delaying medical attention (Markowitz et al. 2017). Dueker et al. (2005) suggest the possibility that physicians may be inclined to reduce their demands for the assistance of nurse practitioners and instead substitute them with physician assistants.
While nonrestrictive SOP laws can have favorable supply and demand repercussions for nurse practitioners, the impact on wages is ambiguous. On one hand, nonrestrictive SOP laws that promote effective collaboration and teamwork (Xue et al. 2016) and eliminate oversight requirement and delays in care (Markowitz et al. 2017) may lead to improved productivity of nurse practitioners. On the other hand, possible directional changes in the labor supply of and demand for nurse practitioners under full SOP laws can have offsetting impacts on the final equilibrium wage level.
Data and Methods
We use data from several sources to evaluate how SOP laws affect nurse practitioners’ labor market outcomes. Our primary data source is the quadrennial National Sample Survey of Registered Nurses (NSSRN), which is a principal source of nationally representative active licensed-to-practice nurse workforce data. It is collected every 4 years by the Health Resources and Services Administration (HRSA) to monitor the trends of the nurse workforce, including nurse practitioners, from 1977 to 2008.2There are approximately 35,000 licensed nurses in each survey. We compiled 6,110 nurse practitioner observations for the period 1980 to 2008. We dropped the survey of year 1977 because it missed key variables focused on in this study. Surveys were conducted by mail and telephone follow-ups, and approximately 75% of the interview requests were responded to. The population of nurses can be compared by year and state because over the years NSSRN incorporated a complex, nested sample frame to ensure equal probability of nurse observation selection in each state.3
The 2008 NSSRN used a sampling design that is slightly different from previous surveys. It introduced adjustment of nonresponse within age group, which further increased the accuracy of national estimates of the nurse population. Meanwhile, the Health Resources and Services Administration (2010) conducted a comparison of 2008 NSSRN sampling methods to previous methods and found very minimal differences between the estimates from the 2008 sample and previous samples, which suggested comparability of the 2008 sample to the previous samples in trend analysis. Sampling weights have been calculated and added to the observation of each nurse in each state. NSSRN provide individual labor market outcome variables such as working hours and wages of nurse practitioners. The dataset also includes a series of valuable individual-level demographic information that could be used to control confounding effects.
Macro-level economic indicators, such as total government spending and health spending per capita, are obtained from the Census of Governments State and Local Finance series. Business cycle variables are extracted from the Bureau of Economic Analysis. Finally, these data are supplemented with information on the number of physicians per 1,000 people and the share of the population over 65 years old from the Area Health Resource Files provided by the Health Resources and Services Administration.
Information on state-level adoption of full SOP laws can be obtained from the Annual Legislation up- dates published by the Nurse Practitioner Journal each year. Moreover, we also use information on full SOP laws compiled by Alexander and Schnell (2019) and Traczynski and Udalova (2018).
Dependent and independent variables
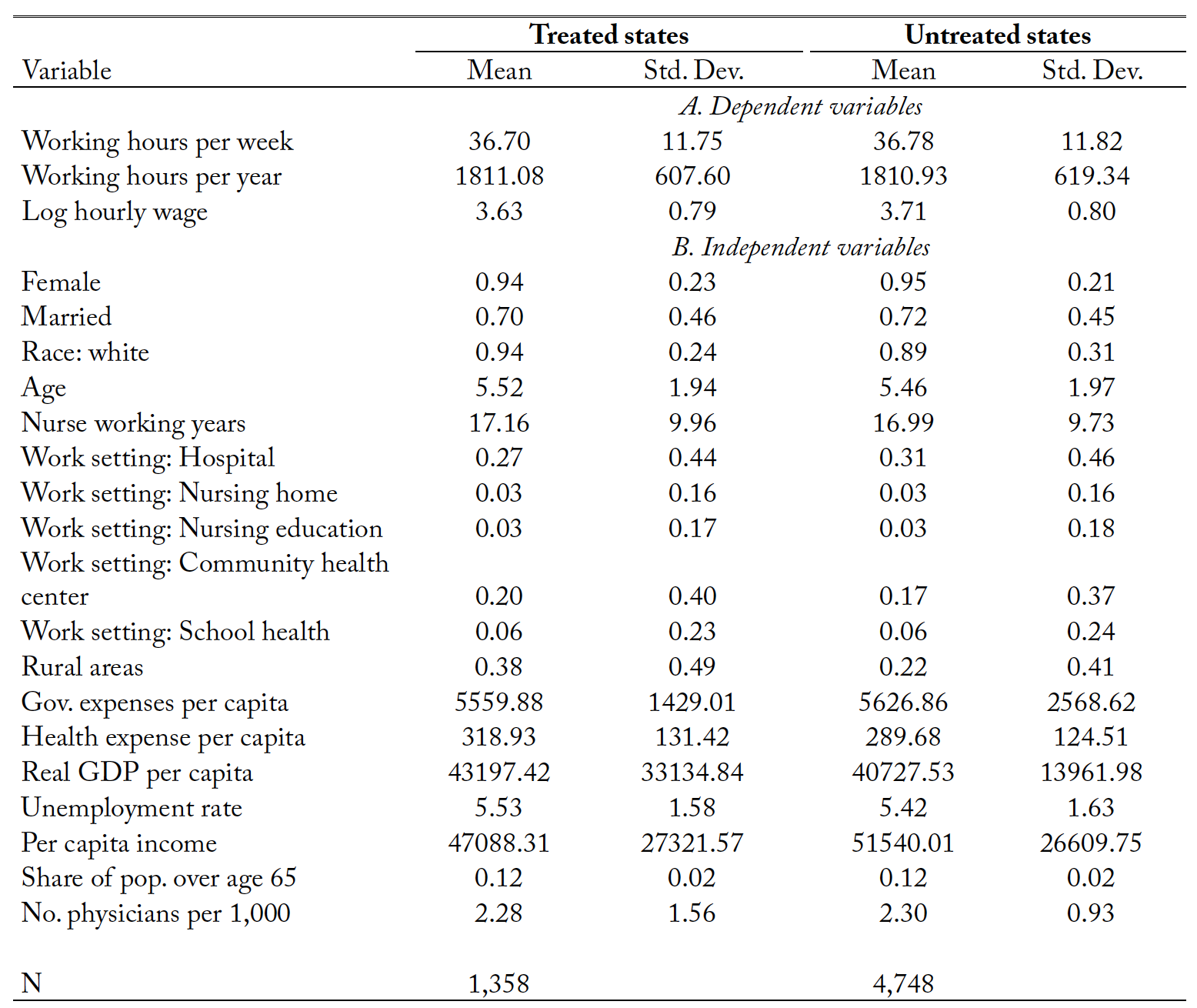
In analyzing the NSSRN data, we define three labor market outcomes for nurse practitioners, namely, (1) working hours per week; (2) working hours per year; and (3) logarithm of hourly wages. Hourly wages of nurse practitioners are calculated by dividing the gross annual salary earnings with the total number of hours worked per year. Table 1 shows the summary statistics for states with and without full SOP.
In addition to the labor market outcomes of nurse practitioners, which are similar between full SOP adopting and nonadopting states, NSSRN data also enables us to examine other aspects of nurse practitioners’ labor supply decisions. These factors include choices of employment settings among such alternatives as hospitals, community health centers, ambulatory care, and other agencies. The nurse practitioners’ task allocation decisions between administrative duties and patient care after gaining professional independence can also be analyzed. In addition, we investigate labor supply responses by examining if more nurse practitioners move into the nonrestrictive states and if registered nurses are more likely to enroll into advanced nursing programs (master or PhD programs) when full SOP laws are enacted.
Included covariates can be divided into three categories: demographic and employment characteristics, macroeconomic indicators, business cycle variables, and other variables.
Demographic characteristics include gender, marital status, race, and age. As can be gleaned from the summary, there is not much difference in such attributes among nurse practitioners in states with full SOP laws and nonadopting states. The majority of nurse practitioners are female, white, in their 30s and 40s, and married. These characteristics mirror the average profile of the nurse practitioner sample in the National Ambulatory Medical Care Survey (NAMCS) as reported by Kurtzman and Simmens (2017). There are no significant differences in their employment characteristics (such as working experience and employment settings) in treated and untreated states.
Table 1. The selected summary statistics for states with and without full SOP laws.
Notes: Statistics are weighted by the survey weight. “Treated states” include states that have adopted full scope-of-practice laws. “Untreated states” have not. “Age” is a variable with ten categories from “Less than 25 Years of AGe” to “65 or More Years of Age.”
Our results, however, indicate that nurse practitioners in treated states are more likely to work (38%) in rural areas than those in untreated states (22%). The same figure for untreated states was obtained Kurtz- man and Simmens (2017) using NAMCS data. Our study thus lends support to the idea that full SOP laws increase services in underserved areas like rural communities.
The states that adopted full SOP laws also have higher per capita health expenditures, which may be related to their residents’ higher health care service utilization rates. Full SOP adopting states and nonadopting states seem to have similar macroeconomic conditions and resource endowment (number of primary physicians per 1,000 population).
Difference-in-Differences Model
The adoption of SOP laws across states on different years provides a quasi-natural experiment that can be explored using a difference-in-differences (DID) model. The specification of the DID model that estimates the impact of full SOP law adoptions are constructed as follows:
(1)
where is the measure of outcomes, such as working hours and wages of nurse practitioners.
equals one if a state gives professional independence to nurse practitioners without requiring physicians’ supervision or collaboration, zero if otherwise.
is a vector of covariates controlled in the model
and
are year and state fixed effects, respectively.
is the error term.
As specification checks, we present the results of the DID model with state-specific time trend, without business cycle covariates and without other control variables. The regressions are weighted by the sample weights provided by the survey to generate nationally representative estimates for nurse practitioners. We also present, along with the main results, estimates obtained from unweighted regression techniques. These robustness checks show that the DID estimates are consistent and reliable.
One crucial assumption of DID estimation is the parallel pretrend assumption, which requires the trends of outcomes between treated and untreated states to be similar and parallel before the event. Thus, in the absence of intervention, the trends should be similar after the cutoff year. If a statistically different gap is found after the cutoff year between treated and untreated states, it can be concluded that the intervention is the cause for the deviations of outcomes in treated states vis-à-vis untreated states’. The event study specification that can be used to test the parallel pretrend is
(2)
The model has leads and
lags. The vector
contains the dynamic impact estimates of SOP law adoption in each year before and after the adoption. We test the assumption that there is no significant difference between the treated and untreated states; thus, the coefficients before the adoption from the pretreatment periods should not be statistically different from zero. Similarly, the number of coefficients that are statistically significant after the adoption can reflect two things: (1) if there is any significant impact and (2) the duration of such impact on the labor market outcomes for nurse.
Full SOP policy exogeneity
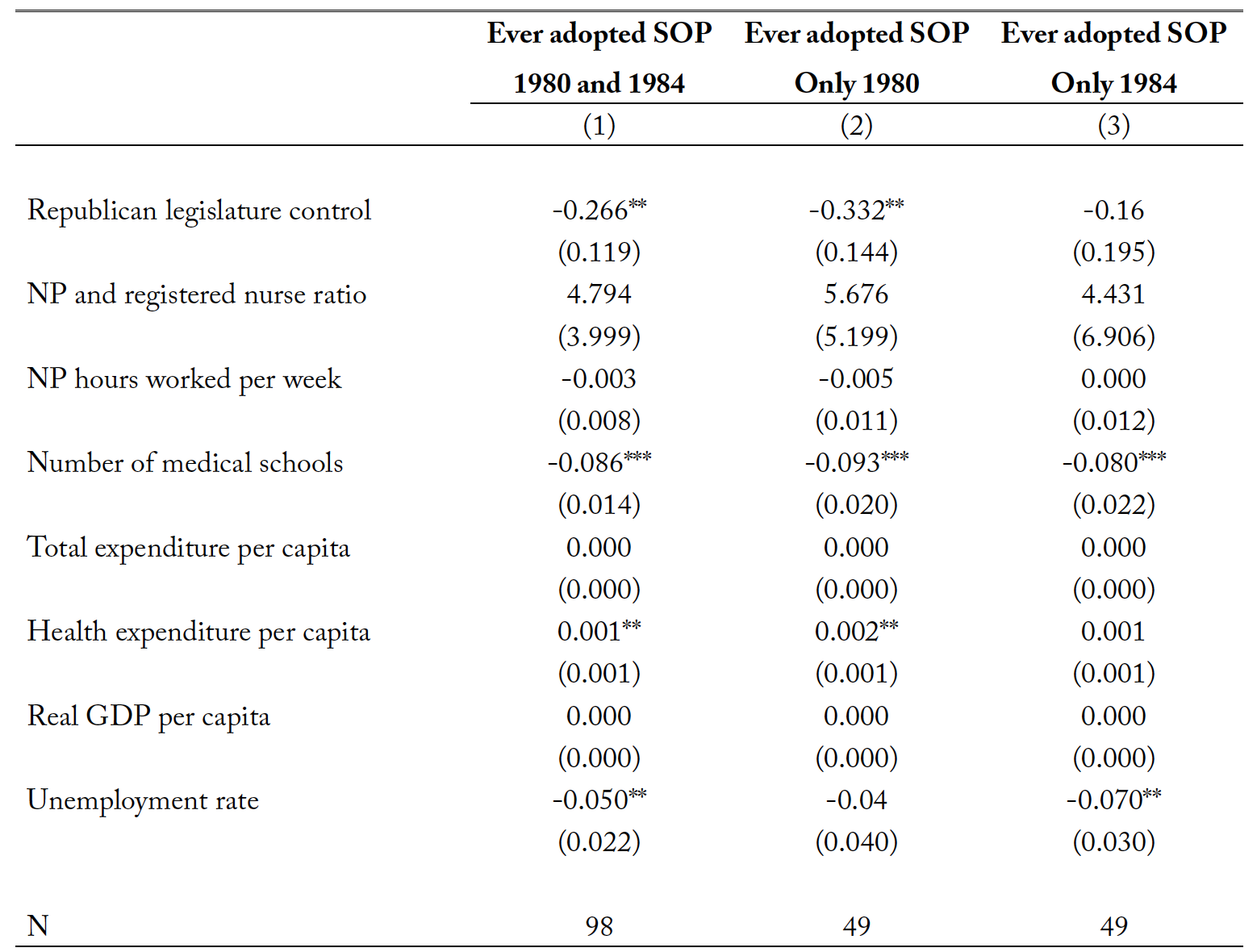
As noted by Traczynski and Udalova (2018) and Markowitz et al. (2017), policy endogeneity may be an issue in SOP-related studies. If the states that adopted SOP laws had previously experienced better or worse labor market outcomes for nurse practitioners, the estimates could be biased. However, Traczynski and Udalova (2018) suggest this actually should not be a concern because a state’s decision to implement SOP laws is usually a result of political bargaining among political appointees, the attorney general’s opinions, and other similar factors. Markowitz et al. (2017) find little evidence of policy endogeneity by testing if the timing of granting prescriptive authority to nurse practitioners is correlated with variables such as county-level health care provider counts or health insurance coverage rate. Their results show that a change in SOP laws is not caused by these indicators. Following Traczynski and Udalova (2018), we look at some determinants in 1980 and 1984 when very few states had adopted SOP laws and check how these factors in the past would have affected the eventual adoption of SOP laws later by more states. The results are presented in table 2.
Estimates in columns (1) to (3) show the results of policy exogeneity tests for samples in different time episodes: 1980 and 1984, 1980 only, and 1984 only. As can be seen, the decisions to adopt full SOP laws later are not determined by the labor supply of health care professionals. Instead, such decisions are influenced by other factors, such as the Republican Party’s control of state legislation. We also find that the proliferation of medical schools in 1980 and 1984 reduced the probability of passing full SOP laws later. Traczynski and Udalova (2018) suggest that the number of medical schools predicts the political power of physicians in a state, which would reduce the incentive for enacting full SOP laws. Moreover, future adoption of full SOP laws can depend on per capita health expenditures and unemployment rate.
Table 2. Determinants of scope-of-practice law adoption across states.
Notes: NP denotes nurse practitioner. SOP denotes scope-of-practice laws. ** p<0.05 and *** p<0.01
The results of table 2 are consistent with those reported by Traczynski and Udalova (2018) and supported by other findings (e.g., Safriet (2002) and Issacs and Jellineck (2013)). These studies conclude that factors such as political connections and fundraising efforts may play a larger role than the labor supply of health care professionals in SOP legislation. Thus, the adoption of full SOP laws can be treated as exogenous.
Empirical Results
Labor market outcomes
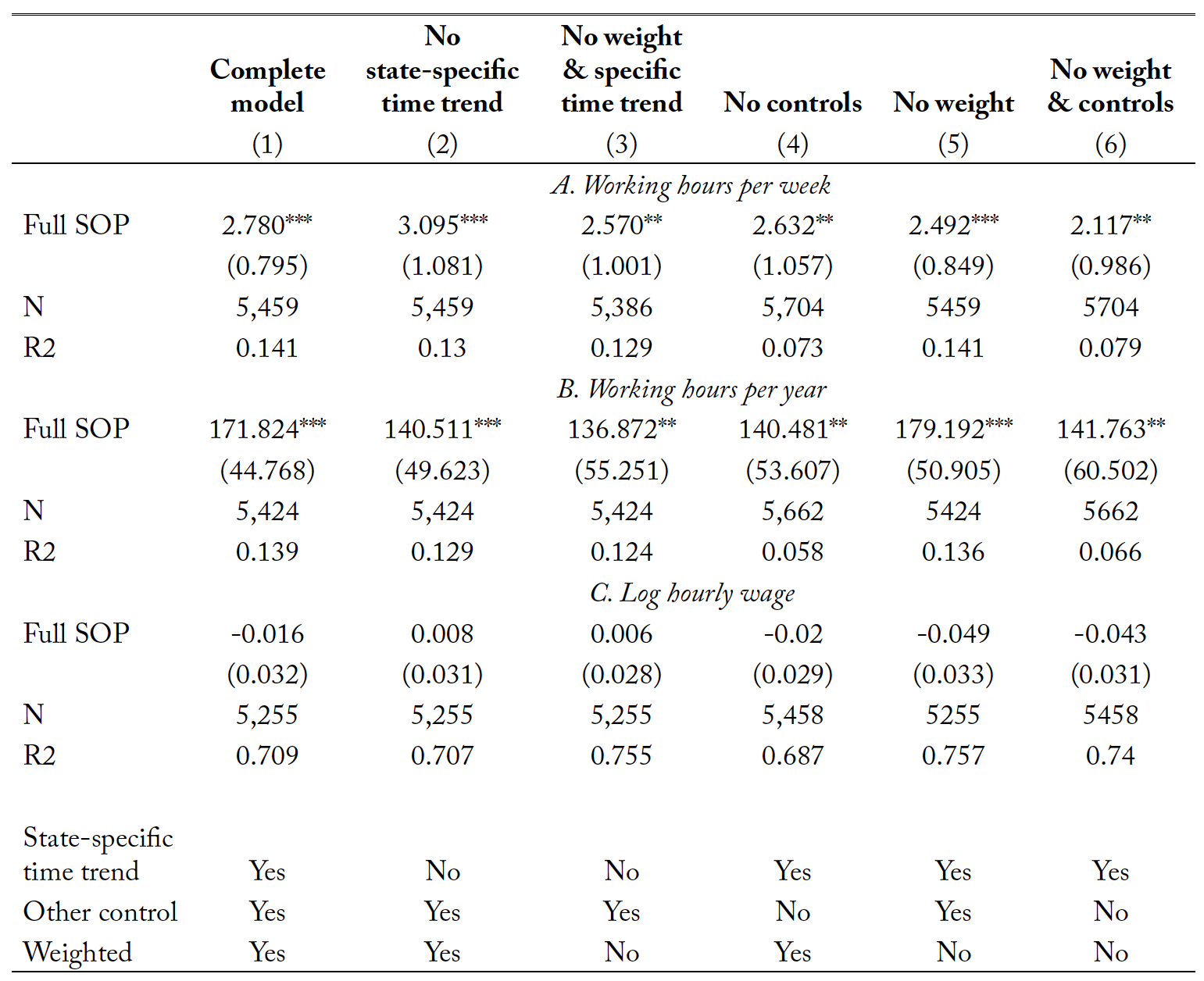
Results in table 3 summarize the labor market outcomes of nurse practitioners after the adoption of full SOP laws. Panels A and B contain results for the number of hours worked per week and per year, respectively. The estimation in column (1) controls for state-specific time trends to address possible correlations arising from coincidences between the introduction of SOP laws and trends in control states that may also affect labor supply decisions of nurse practitioners. In addition, the inclusion of state-specific linear time trends addresses the concern that some temporal gaps in the data could be driving the results. Angrist and Pischke (2008) point out that the inclusion of such trends indeed leaves the estimated effects of interest unchanged. Results in column (2) show that full SOP laws increase nurse practitioners’ work-time allocation by 2.78 hours per week and 171.8 hours per year. These results are significant at the 1% level. As can be seen from column (2), which excludes state-specific time trends, granting practice and prescription independence to nurse practitioners would increase their working hours by about 3.1 per week and 140.5 per year. The estimates in both columns are consistent; a t-statistic value of 0.414 indicates that they are not statistically different from each other.
Specification check results in columns (3) and (6) also provide robust evidence supporting the conclusion of an increased work-time allocation trend. Solon, Haider, and Wooldridge (2015) suggest reporting both weighted and unweighted estimates because consistent parameters of these two indicate a correctly specified model. In this analysis, the estimates in columns (3), (5), and (6) obtained from a regression without survey’s sample weights slightly change compared to the estimates in columns (1) and (2), but they are still broadly in line with the conclusions.
The findings on changes in work-time allocation are in line with results of previous research. Kleiner et al. (2016) find that required supervision from physicians would reduce the annual working hours of nurse practitioners by approximately 219 hours, thereby clearly preventing nurse practitioners from providing better service to their patients. Cai and Kleiner (2016) examine the effect of restrictive regulation on occupational therapists and physical therapists and find reductions in annual working hours by 47.07 and 43.2 hours, respectively. However, Timmons, Hockenberry, and Durrance (2016) provide suggestive evidence showing that expanded SOP would reduce the working hours of chiropractors by 1.108 hours per week.
They explain that the expanded SOP enables chiropractors to charge higher prices for their services, thus they are able to afford fewer working hours. The result that full SOP laws increase the working hours of nurse practitioners is consistent with the prediction of the conceptual framework that more professional independence and increased medical needs would incentivize nurse practitioners to provide more services.
Results in panel C show hourly wage outcomes of SOP laws for nurse practitioners. Estimates in panel C indicate that full SOP laws do not have any significant impact on the hourly wages of nurse practitioners. Cai and Kleiner (2016) also find that occupational licensure would not affect the wage of occupational therapists who are authorized to have more autonomy to practice physical therapy. Full SOP laws increase the labor supply of nurse practitioners and therefore impose a downward pressure on their wage level.
However, given the burgeoning demand for health care services and the competition dynamics in health care markets in the country, the wage markdown effect of increased supply could be offset by the high demand for nurse practitioners’ services. In addition, patients are actually more willing to pay higher prices for nurse practitioners’ services, because the adoption of expanded SOP regulations acts as a signal of their quality (Timmons, Hockenberry, and Durrance 2016). Moreover, as suggested in the conceptual framework, eliminated oversight requirements and improved teamwork efficiency (Xue et al. 2016; Markowitz et al. 2017) may also increase the productivity of nurse practitioners and help restore their wage to its original level.
An additional explanation for the unchanged wage level could be a concentration shift in their job responsibilities. When nurse practitioners are given professional independence, they could be inclined to allocate more time to administration instead of patient care. Patient care services may become costlier under an expanded SOP scenario but administrative assignments may not offer a change in employees’ marginal returns. As a result, nurse practitioners who devote most of their increased working hours to administrative tasks instead of patient care would not experience any change in their hourly wage level. We provide evidence to support the argument of changing concentration among job responsibilities in table 6.
Table 3. The results of full scope-of-practice laws for the labor market outcomes of nurse practitioners.
Notes: Full SOP denotes a full scope-of-practice law that grants full independence to nurse practitioners. Other controls included in the OLS regressions are gender, marital status, race, age, experience, employment settings, rurality, government expenses per capita, health expenses per capita, real GDP per capita, per capita income, unemployment rate, share of population over age 65, number of active medical doctors per 1,000 population, year fixed effect, and state fixed effects. All regressions are weighted by the sample weight provided by Nursing Workforce Survey. ** p<0.05 and *** p<0.01.
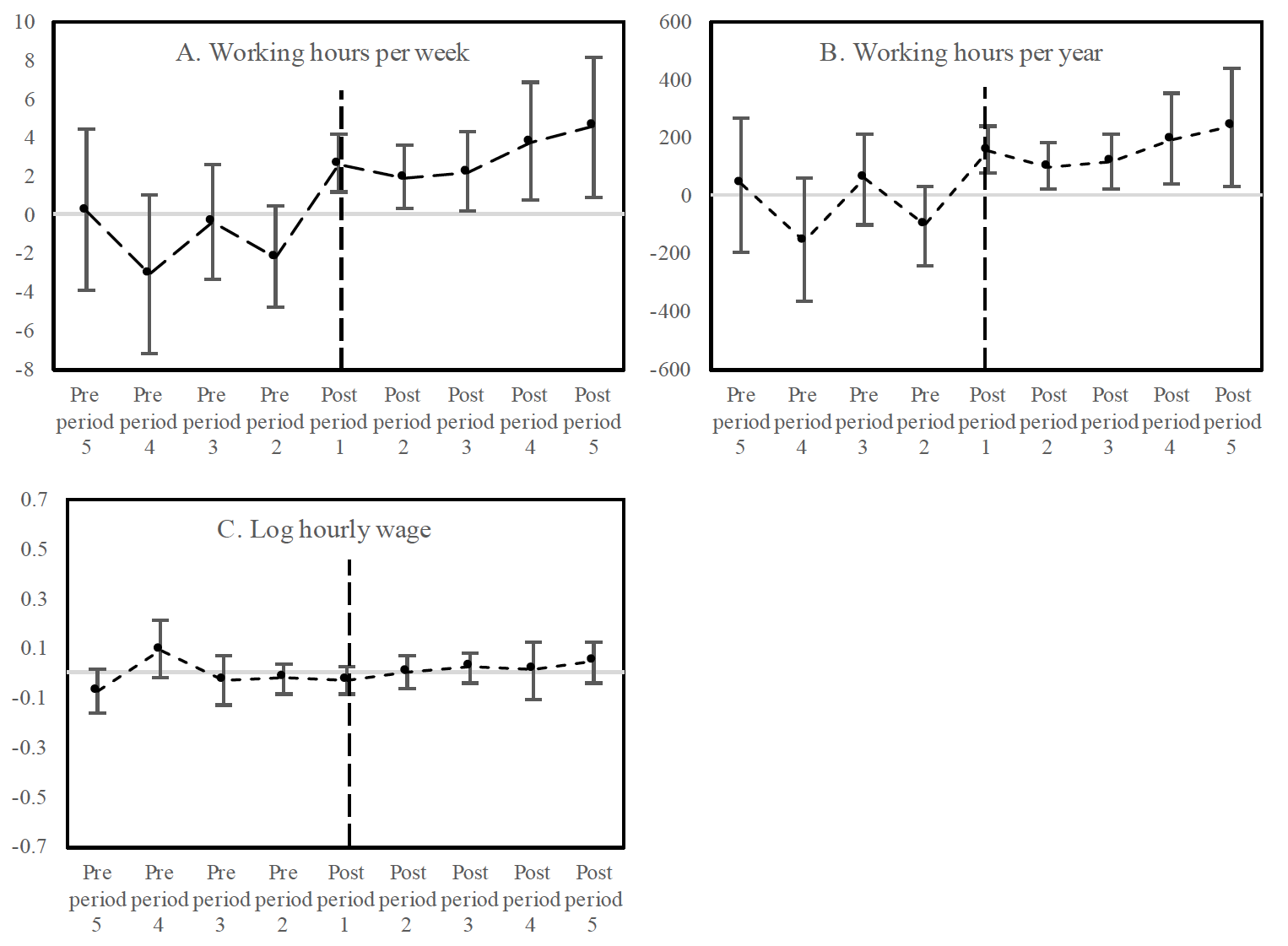
Event study estimates
The reliability of DID estimates depends on the parallel pretrend assumption that the differences in outcomes between treated and untreated states are not statistically different from zero during the pretreatment periods. The event study model, as shown in equation (2), can provide empirical evidence to address a concern that the SOP change indicator is simply picking up pre-existing trends in outcome variables. It also helps examine the length of the impact of full SOP laws after the initial adoption. Plots A to C show event study estimates for each year before and after full SOP adoption (figure 3).
Estimates for the pre-adoption years (years before the dashed vertical line) are not statistically different from zero across the plots in figure 3. In fact, most of the coefficients for the pretreatment periods are negative and not statistically significant. This means that there is no significant difference in outcomes between treated and untreated states during pretreatment periods; this therefore suggests parallel trends. The estimates change after the adoption line and we can see notable increases in the impacts of full SOP laws. Most of these changes, particularly for the working hours per week and per year, are statistically significant from zero in plots A to C. As a result, we can say that full SOP laws increase the nurse practitioners’ number of working hours. Moreover, the upward trends of working hours persist through the post-treatment years. This suggests that the effects of full SOP laws are not short-lived but persistent for a while. The long-lasting impact on employment outcomes of nurse practitioners may substantially change the health care provision landscape in the long run.
Figure 3. The dynamic estimates of full SOP laws’ impacts on nurse practitioners.
On the other hand, we do not see any statistically significant estimates of full SOP laws on the hourly wage levels during the post-treatment period (plot C). The event study estimates further corroborate the main findings.
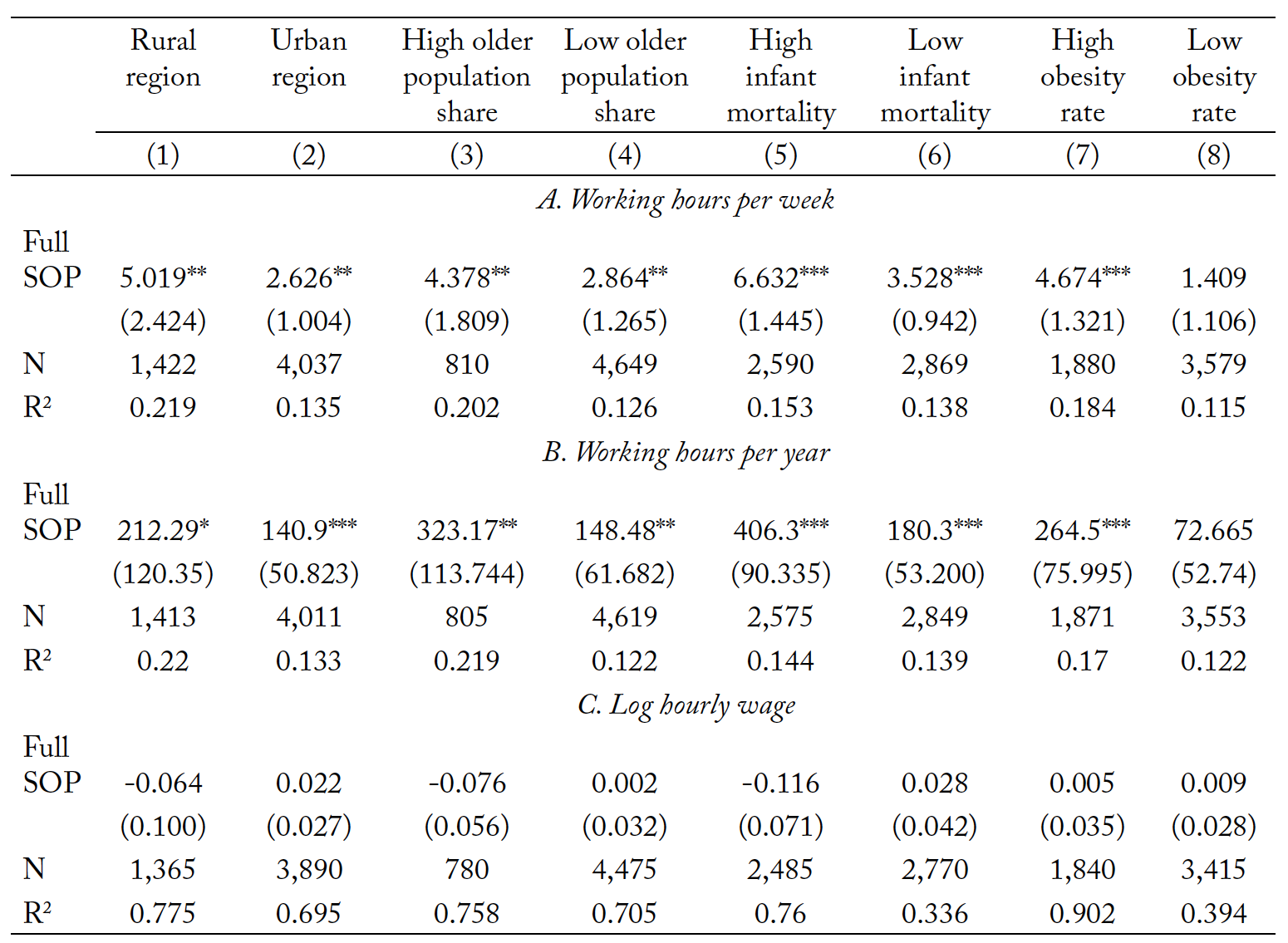
Heterogeneity analysis
Heterogeneity analysis would help pinpoint areas of work where nurse practitioners would devote more of their working times and what subpopulations could benefit from expanded SOP laws. Moreover, heterogeneity analysis applied to people with different medical needs could provide information on the impact of SOP laws from the demand side. Expanded SOP laws that lead nurse practitioners to provide quality services could have a more prominent influence in areas with more serious public health concerns. We divide the sample according to rurality, share of population who are 65 years and older (<14% vs. >=14%), infant mortality rate (<8 vs. >=8 per 1000 live births), and obesity rate, which is determined by the percentage of the adult population reporting a body mass index (BMI) greater than or equal to 30 (<25% vs. >=25%). The sample is divided based on their median value.
Health disparities exist between populations living in urban and rural areas (Sonenberg and Knepper 2017). The life expectancy of the rural population (76.8 years) is two years shorter than the urban population (78.8) in the U.S. (Meit et al. 2014). If professional autonomy can encourage nurse practitioners who are in rural areas to work more hours, it could help close the gap in health outcomes between urban and rural populations.
Table 4. The heterogeneity analysis of the impacts of full SOP laws.
Notes: Full SOP denotes a full scope-of-practice law that grants both practice and prescription independence to nurse practitioners. High older population share denotes the states with more than 14% of the population who are older than 65 years old. High infant mortality denotes the states with an infant mortality rate higher than 8. High obesity rate denotes the states with obesity rate higher than 25. Covariates included in the difference-in-differences model are gender, marital status, race, age, experience, employment settings, rurality, government expenses per capita, health expenses per capita, real GDP per capita, per capita income, unemployment rate, share of population over age 65, number of primary care physicians per 1,000 population, year fixed effect, and state fixed effects. All regressions are weighted by the sample weight provided by the Nursing Workforce Survey. * p<0.1, ** p<0.05m and *** p<0.01.
Results in columns (1) and (2) show that nurse practitioners working in urban areas increase their working time by about 2.6 hours per week and 140.9 hours per year. One of this study’s compelling results is evidence of a more notable increase of 5.1 working hours among nurse practitioners in rural areas. The annual working hours of rural nurse practitioners also record larger increments than urban nurse practitioners, though the estimate is significant only at the 10% level. This finding is in line with our expectation that full SOP laws would increase the working hours of nurse practitioners in rural areas. This is also consistent with the results of previous studies (e.g., Xue et al. (2018), Ortiz et al. (2018), Grumbach et al. (2003), and Newhouse et al. (2011)), which show that expanded SOP laws increase the labor supply of nurse practitioners in rural areas and improve the health status of the rural population. The findings of increased working time further bolster the claim that practice and prescription authority would enhance health care service access in rural areas by making nurse practitioners more available. Given the limited medical service access for residents in rural communities (Shin et al. 2012), an increased labor supply could fill in the supply gap of health professionals in these areas. Increased access to primary care would improve health equity between the urban and rural regions (Chetty et al. 2016).
Results from columns (3) to (8) show the impacts of full SOP laws on groups with different medical care needs. As can be seen, regions with a higher share of population who are 65 years and older, infant mortality rate, and obesity rate are more likely to see a larger increase in working hours of nurse practitioners compared to regions with fewer medical needs. The results point to the same conclusion as the results in columns (1) and (2) that full SOP laws would encourage nurse practitioners to serve those who are in greater need. Conversely, populations in medical shortage areas increase their demands of and visits to nurse practitioners after the adoption of full SOP laws. A more prominent increase in working hours of nurse practitioners in areas with more serious health issues also suggests that there are unmet medical needs in some regions in the U.S. Finally, the results in panel C table 4 show little change in the wages of nurse practitioners.
Employment setting changes
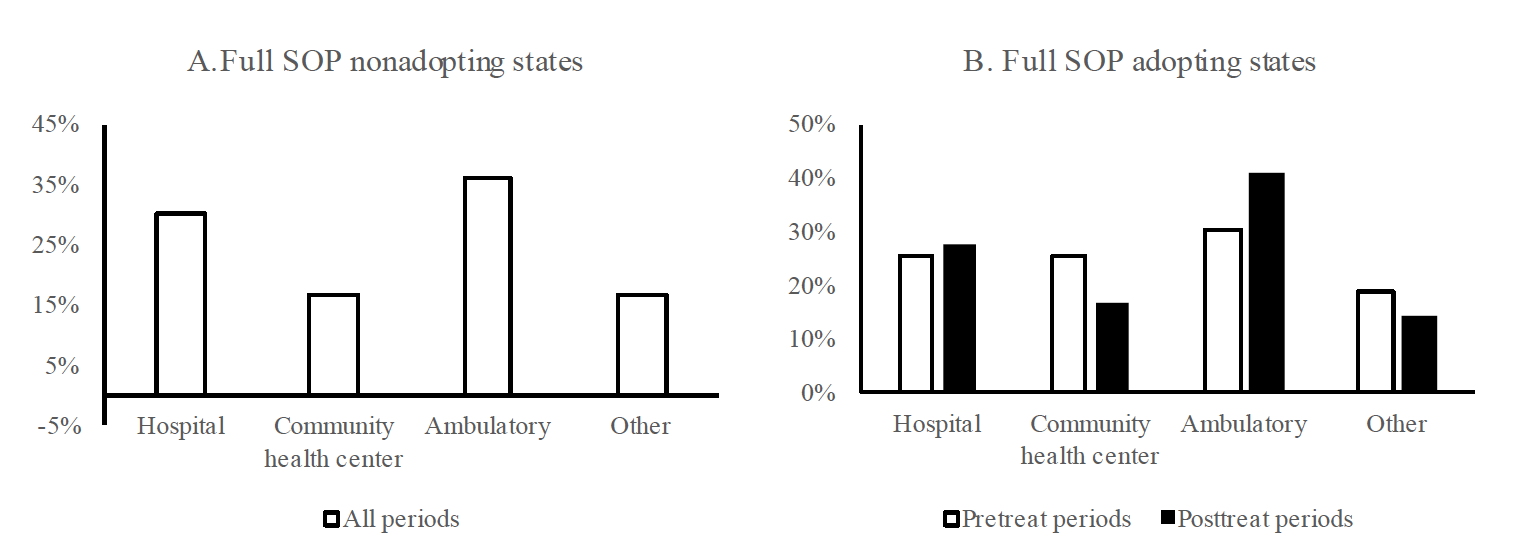
This section investigates how the employment settings of nurse practitioners change after the adoption of full SOP laws. Figure 4 shows the share of nurse practitioners in different employment settings, such as hospitals, community health centers, ambulatory care agencies, and other venues (e.g., nursing education, nursing home, school health, and occupational health). The shares are calculated based on the sample data of NSSRN. In contrast to hospitals and community health centers, ambulatory care agencies provide personal health care services that do not involve overnight stays. As can be seen from plots A and B in figure 4, the majority of nurse practitioners are employed in ambulatory care agencies, followed by hospitals and community health centers. About 15% of them work in other health care institutions.
Figure 4. Distribution of nurse practitioners across employment settings in full SOP adopting and nonadopting states.
We find some changes in the shares of nurse practitioners working in different health care agencies before and after full SOP adoption in plot B. As can be seen, the share of nurse practitioners working in community health centers decreased from 25.2% to 16.9% after the adoption. Meanwhile, the share of nurse practitioners working in ambulatory care agencies increased from 30.3% to 40.8% after the adoption. There is a slight decrease in the share of nurse practitioners working in other employment settings, except for hospitals where the change was at most minimal.
To explore the employment setting changes, we utilize information on each nurse practitioner’s employment settings including hospital, community health center, ambulatory care agency, and other agencies. A nurse practitioner reports to work in one principal employment setting. The specification of the regression is constructed as follows:
(3)
where is a categorical outcome that shows the employment settings.
equals one if a state grants professional independence to nurse practitioners without requiring physicians’ supervision or collaboration, zero if otherwise.
is a vector of covariates controlled.
and
are year and state fixed effects, respectively.
is the error term. Due to the categorical nature of the employment setting variable, we use multinomial logit regression within the DID model. The results are presented in table 5.
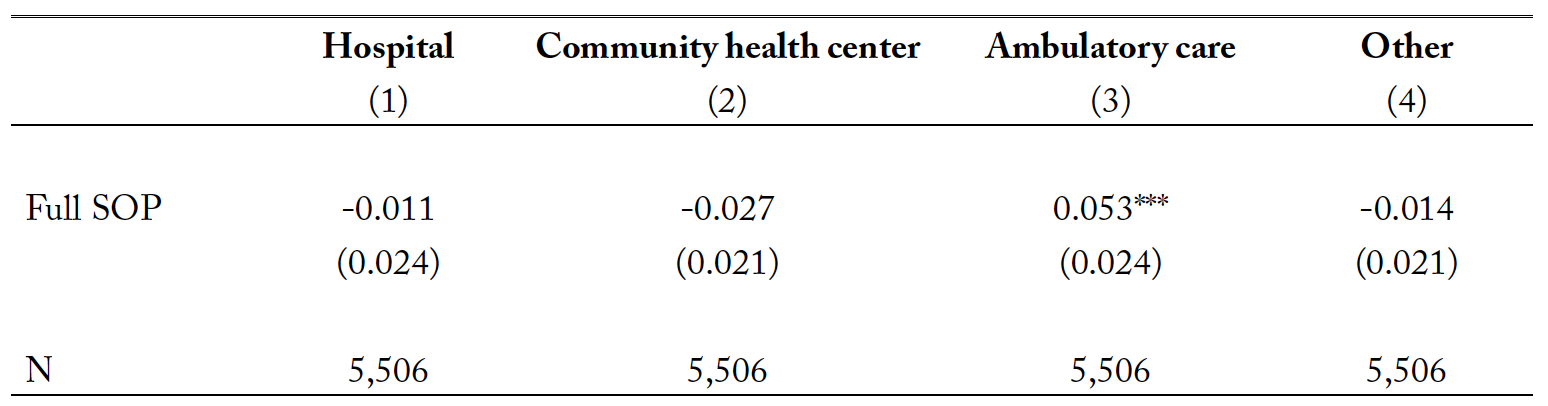
Table 5. The estimated impacts of full SOP laws on the employment settings of nurse practitioners.
Notes: Full SOP denotes a full scope-of-practice law. Covariates included in the multinominal logit DID model are gender, marital status, race, age, rurality, total government expenditure per capita, real GDP per capita, unemployment rate, share of population 65 years and older, year fixed effect, and state fixed effects. All regressions are weighted by the sample weight provided by the survey. ** p<0.05 and *** p<0.01.
The estimate in column (3) shows that the probability of working in an ambulatory care agency increases by about 5.3 percentage points. However, estimates for hospital, community health center, and other health care agencies were not statistically significant. The higher likelihood of working in ambulatory care reflects the great demand for acute care nursing services (Dueker et al. 2005), a category befitting ambulatory care services patronized by most people receiving medical care in the U.S. (Rondinelli et al. 2014). This likelihood also can be due to the compensation structure of ambulatory care services, which registered the highest wage level at $58.81 per hour. Our data also show that nurse practitioners in community health centers have the lowest hourly wage at $39.43. It is therefore logical to see a decreased share of nurse practitioners working in community health centers after they gained professional independence.
Additionally, nurse practitioners are more likely to function in both alternative and complementary roles to primary care physicians in an ambulatory care setting. Nurse practitioners who play alternative roles provide similar services as those obtained from primary physicians. In their complementary capacity, nurse practitioners provide additional or extended services that do not duplicate primary physicians’ services (Martin-Misener et al. 2015).
Hospitals, private physician practices, and community health centers usually have nurse practitioners working under the direct oversight of physicians. As a result, nurse practitioners with full SOP in these agencies may find it difficult to practice independently due to the restrictive relationship with their supervisors and aggravated possibly by the competitive atmosphere between them and physicians. Ambulatory care agencies are employment settings where nurse practitioners are equally cost-effective and can provide similar alternative quality services (Dierick‐van Daele et al. 2009; Kinnersley et al. 2000; Mundinger et al. 2000), and thus these settings could attract more nurse practitioners with practice and prescription authority.
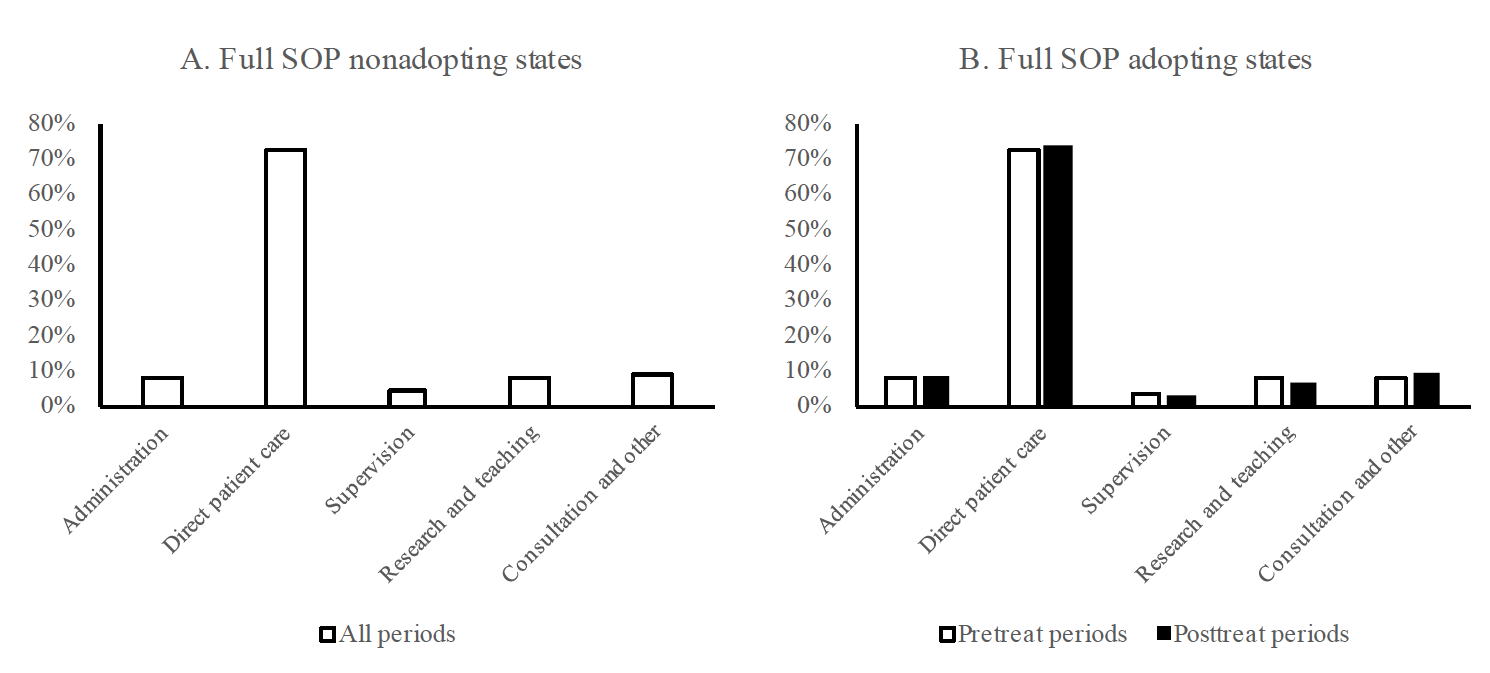
Task changes
Full SOP laws affect not only the employment settings of nurse practitioners but also the specific tasks they perform. Figure 5 shows the proportion of time nurse practitioners devote to each type of task from the calculation based on NSSRN data. As the trends indicate, nurse practitioners assign over 70% of their working time to direct patient care. Plot B shows that nurse practitioners in states with full SOP laws experienced a slight increase in the share of time devoted to patient care after the adoption. That increase is not statistically significant.
Nurse practitioners who can practice and prescribe independently also would assume more administrative tasks as they may establish and run their own clinics. However, plot B shows minimal change in the share of time for administrative work before and after the full SOP laws in both adopting and nonadopting states.
Consultation is another important task for nurse practitioners, because their training is specifically geared toward patient consultation, education, and providing professional advice on the management of acute and chronic illness as well as preventive care (DeAngelis 1994). As suggested by previous studies, nurse practitioners provide more consultation related to preventive care and health risk behavior counseling than physicians do (Moody, Smith, and Glenn 1999; Hooker and McCaig 2001). With greater professional independence, nurse practitioners may take full advantage of their training and focus more on providing consultation and preventive care that could distinguish their services of specialty from physicians’ services. The share of time devoted to consultation in adopting states increases in plot B, thus suggesting that nurse practitioners have enhanced their consultation roles. Plot B in figure 5 also shows that full SOP adopting states witness decreases in time allocated to supervision, research, and teaching among nurse practitioners. As full SOP laws grant nurse practitioners greater practice and prescription autonomy, they may move away from their roles of supervising other health professionals and assume tasks that take full advantage of their training.
Figure 5. Function changes of nurse practitioners in full SOP adopting and nonadopting states.
We utilize NSSRN data to investigate the impact of full SOP laws on the number of hours allocated by nurse practitioners to different tasks. The dependent variables are the total number of hours assigned by a nurse practitioner to tasks including administration, direct patient care, supervision, research and teaching, and consultation and other. We run a regression for each task using the model specified as follows:
(4)
where is a continuous outcome showing the number of hours devoted to each task by a nurse practitioner.
equals one if a state grants professional independence to nurse practitioners without requiring physicians’ supervision or collaboration, zero if otherwise.
is a vector of covariates.
and
are year and state fixed effects, respectively.
is the error term. Because the assignment of time to these tasks by a nurse practitioner could be correlated, we employ seemingly unrelated regressions to explore the decisions of hours assigned to each task by nurse practitioner in the wake of full SOP adoption. The results are shown in table 6.
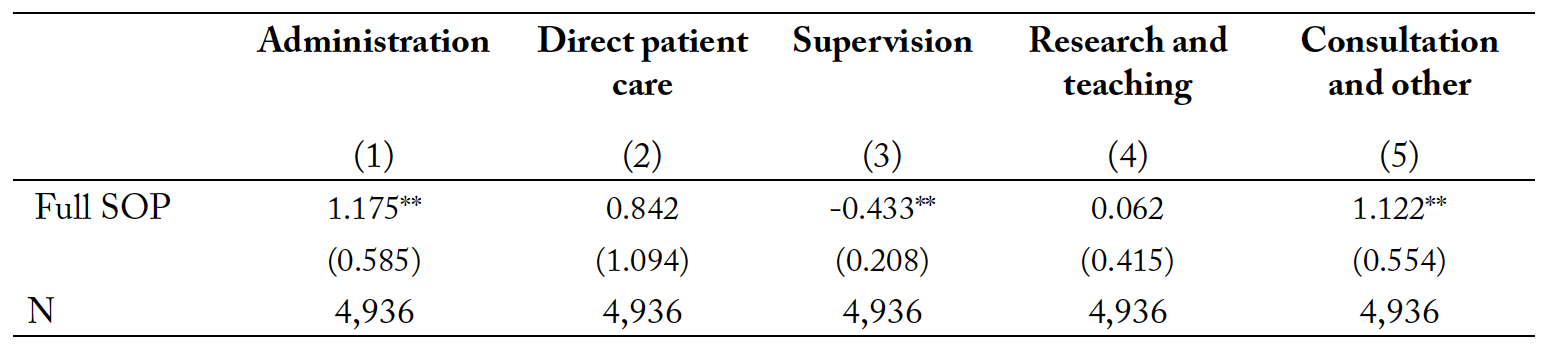
Table 6. The impacts of full SOP laws on working time allocation across tasks of nurse practitioners.
Notes: Full SOP denotes a full scope-of-practice law. Covariates included are gender, marital status, race, age, experience, employment settings, rurality, government expenses per capita, health expenses per capita, per capita income, unemployment rate, number of primary care physicians per 1,000 population, year fixed effect, and state fixed effects. All regressions are weighted by the sample weight provided by the NSSRN. ** p<0.05 and *** p<0.01.
Column (1) in table 6 shows that the time spent on administration increases by about 1.17 hours per week for nurse practitioners after the adoption. Nurse practitioners assume more administrative tasks because they may open their own clinics or practice independently in community health centers and hospitals. In contrast, time spent on supervision decreases by about 0.43 hours per week.4Supervision tasks are assumed by nurse practitioners when they are working for a physician and are required to give guidance and instructions to other health care workers, such as registered nurses. We do not find significant changes in the time devoted to patient care. Increased independence of nurse practitioners may not directly affect the amount of hours devoted to patients but may improve their welfare indirectly, given patients’ need for greater access to primary medical services. The unaffected direct patient care hours support our earlier explanation for the unchanged wage level of nurse practitioners, whereby full SOP laws may lead nurse practitioners to devote more time to administration instead of direct patient care for the sake of realizing increments in their wage level.
The result in column (5) table 6 shows that nurse practitioners increase the time devoted to consultation by about 1.12 hours. This finding is consistent with our earlier prediction that nurse practitioners may shift to tasks that would take full advantage of their training, thereby increasing their competitiveness relative to physicians. In addition, the finding of increased hours in consultation also is consistent with the previous finding (table 5) on their move toward ambulatory care tasks. As suggested by Lin et al. (2004), nurse practitioners play a very significant role in the delivery of health consultation services in ambulatory care settings.
Finally, it can be seen from the results in table 6 that the aggregate number of additional time in ad-ministration and consultation (2.29 hours) supports the main findings in table 3 that nurse practitioners increase their working hours per week by about 2.78. It seems that nurse practitioners would rather prioritize work-time allocation to tasks that further promote their professional independence and optimally utilize their acquired skills, instead of devoting more time to the more essential direct patient care services.
Registered nurses and advanced program enrollment
Restrictive SOP measures may discourage many registered nurses from considering professional advancement to nurse practitioner status (Adams and Markowitz 2018). Moreover, previous studies (Martsolf and Kandrack 2017; Yang et al. 2020) point out that the increased supply of nurse practitioners in expanded SOP states could be partly due to the higher enrollment rates among registered nurses. So far there is only one study (Kalist and Spurr 2004) that examines the impact of SOP regulation on registered nurses’ enrollment into master’s or PhD programs. Their findings indicate that expanded SOP would bring about 12% higher enrollment per capita in advanced programs among registered nurses.
In this analysis, we replicate the approach employed by Kalist and Spurr (2004) that uses the number of total enrollment data from the National League for Nursing (NLN) data until 1995. In our validation, we utilize individual-level data from the NNWS from 1980 to 2008 to investigate if a registered nurse is more likely to enroll in a master’s or PhD program in states with full SOP regulations. Moreover, we investigate if registered nurses with higher skill levels have a higher probability of enrolling in advanced nursing programs after adoption of full SOP laws. As suggested by Traczynski and Udalova (2018), if greater independence in practice attracts higher-ability registered nurses to become nurse practitioners, it would allay the concerns of physician groups of expanded SOP and increase the productivity of the health care sector. Educational attainment and work experience are usually used to measure skill level (Borjas, Grogger, and Hanson 2008). Since most registered nurses are college graduates, we use the years of experience since first obtaining their licenses as an indicator for skill. We also introduce an interaction term between the skill level and the full SOP law indicator to determine if full SOP laws encourage more able and skilled registered nurses to enroll in advanced nursing programs and become nurse practitioners. The basic DID specification is presented in equation (5).
(5)
where is a binary outcome that has value of one if a registered nurse is now enrolled in a master’s or PhD program that usually provides a path to advanced practice nurse career.
equals one if a state grants professional independence to nurse practitioners without requiring physicians’ supervision or collaboration, zero if otherwise.
is a vector of covariates.
and
are year and state fixed effects, respectively.
is the error term. Linear probability model estimates are reported in table 7 as they are similar to the probit model estimates.
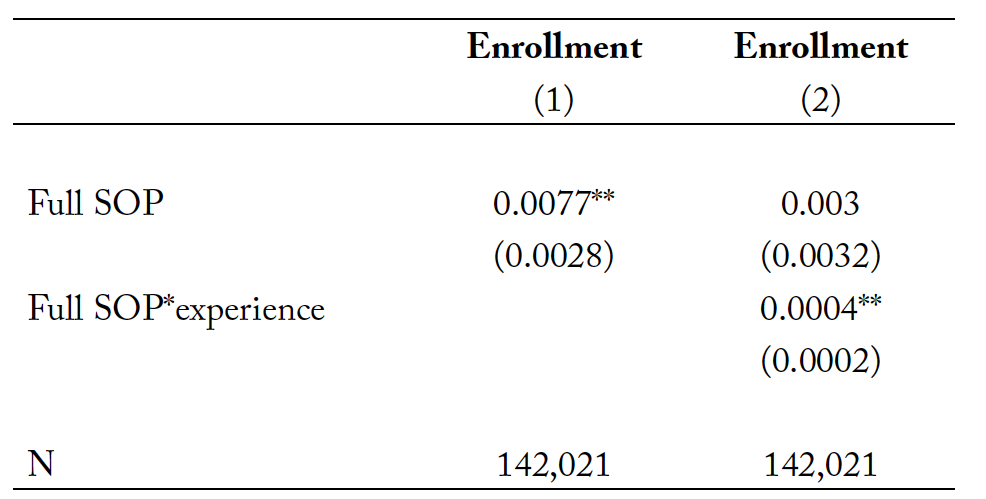
Table 7. The impacts of full SOP laws on the master’s and PhD program enrollment decisions of registered nurses.
Notes: Full SOP denotes a full scope-of-practice law. Covariates included are gender, marital status, race, age, experience, employment settings, rurality, government expenses per capita, health expenses per capita, per capita income, unemployment rate, number of primary care physicians per 1,000 population, year fixed effect, state fixed effects, and the state specific time trend. All regressions are weighted by the sample weight provided by the Nursing Workforce Survey. ** p<0.05 and *** p<0.01.
As can be seen from the results in column (1) of table 7, full SOP laws increase the probability of registered nurses enrolling in advanced graduate programs by about 0.8 percentage points. Given that the ratio between nurse practitioners and registered nurses is 0.043 on average (calculated based on our sample), an increase of 0.8 percentage points is a substantial increase in the future labor force of nurse practitioners.
Moreover, we find evidence showing that full SOP laws would lead registered nurses who are more skilled and have higher ability to enroll in advanced nursing programs. This finding is encouraging because it means that greater professional autonomy for nurse practitioners would not only lead more registered nurse to become nurse practitioners, but also would improve the quality and productivity of this professional group. This ultimately translates to enhanced delivery of services to meet the medical needs of patients while realizing cost savings in the long term.
Migration
Adams and Markowitz (2018) suggest that restrictive SOP laws lead nurse practitioners to move to states with favorable practice environments. Traczynski and Udalova (2018) express similar concerns that they cannot rule out the possibility of nurse practitioners moving into a state with an expanded SOP. However, Traczynski and Udalova (2018) also point out that such movement may be minimal considering the findings of Timmons (2013) on the low mobility rates among registered nurses even when states relaxed barriers to practice across states in the wake of the Nurse Licensure Compacts reform.
This study has two motivations for examining the movement of nurse practitioners across states. First, examining the mobility of nurse practitioners across states could further complement our findings of the labor supply outcomes of nurse practitioners in response to expanded SOP laws. Second, if there is indeed a large-scale movement across states, the estimates of working time in this study may be either overestimated or underestimated, depending on the direction of the movement. Therefore, a check on the movement tendencies of nurse practitioners would corroborate our main results.
We use information from the NSSRN pertaining to the survey question asking nurse practitioners about their geographical state of employment during the year of survey and in the previous year. The specification is shown in the following equation (6).
(6)
where is a binary outcome that equals one if a nurse practitioner indicates he/she migrated from another state in the prior survey year; zero otherwise.
equals one if a state grants professional independence to nurse practitioners without requiring physicians’ supervision or collaboration, zero if otherwise.
is a vector of covariates.
and
are year and state fixed effects, respectively.
is the error term. Results from equation (6) could provide evidence showing if a full SOP state is more likely to have nurse practitioners who migrated from other states after the law’s adoption.
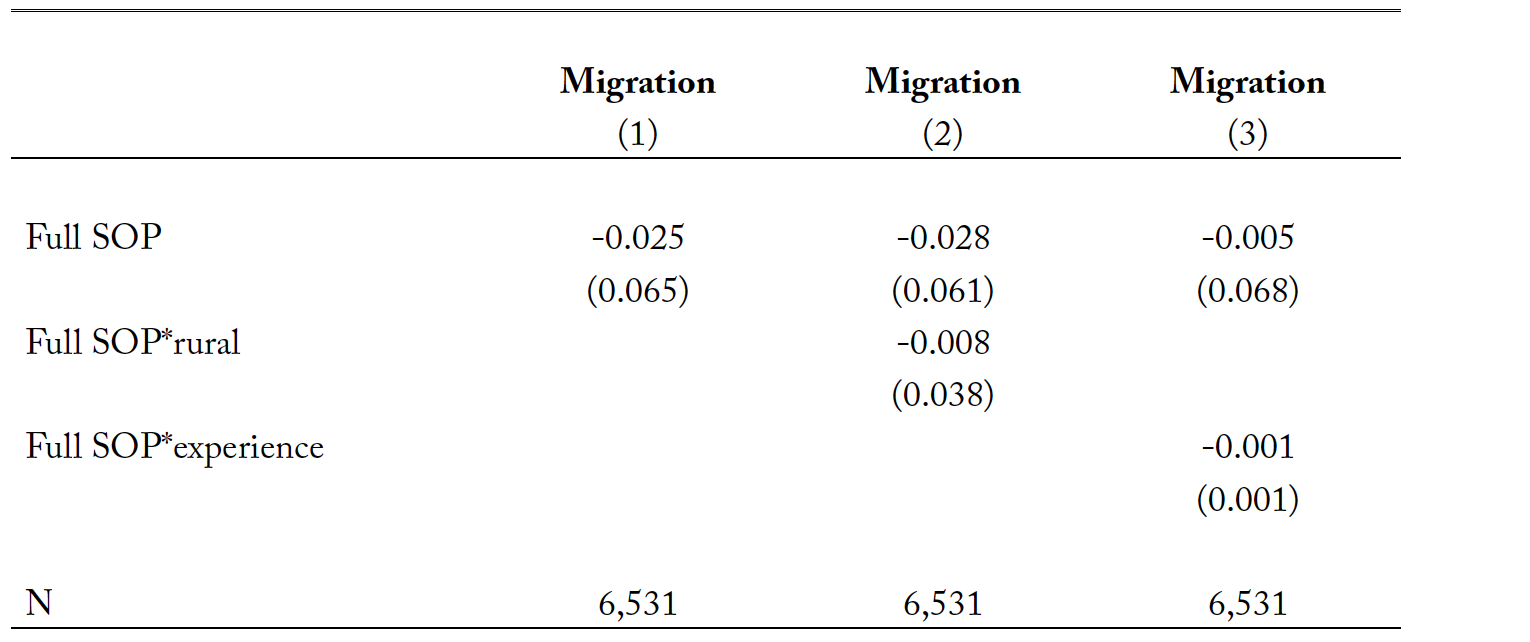
The linear probability model coefficients of the full SOP indicator will indicate the impacts of full SOP laws on the migration of nurse practitioners. Moreover, to reveal if full SOP laws encourage nurse practitioners with high motivations (e.g., nurse practitioners with better ability or those working in rural areas) to migrate to nonrestrictive states, we introduce interaction terms between full SOP laws and rurality as well as skill level which is measured by the working year experience. The results are reported in table 8.
Results in table 8 for different specifications point to the same conclusion: the adoption of full SOP laws does not affect the migration likelihood of nurse practitioners. The results indicate that there is no statistically significant migration tendency among nurse practitioners to migrate to adopting states after the adoption of full SOP laws. Moreover, we also find little migratory responses among nurse practitioners who are more experienced or serving in rural areas. The summary statistics show that over 70% of all nurse practitioners are married, thus inter-state migration decisions are usually made as a family decision and determined by other factors not solely linked to the favorability of the practice environment in full SOP adopting states. However, we would like to mention that due to data limitations, we cannot observe nurse practitioners who migrated into full SOP states beyond the survey’s time period. Moreover, we could neither observe the long-term migratory responses of nurse practitioners nor identify where nurse practitioners migrated from. This could be delegated to future research when data that are more relevant would be available.
Table 8. The impact of full SOP laws on the migration decisions of nurse practitioners.
Notes: Full SOP denotes a full scope-of-practice law. Covariates included in the difference-in-differences model are gender, marital status, race, age, experience, employment settings, rurality, government expenses per capita, health expenses per capita, per capita income, unemployment rate, number of primary care physicians per 1,000 populations, year fixed effect, state fixed effects, and state specific time trend. All regressions are weighted by the sample weight provided by the Nursing Workforce Survey. ** p<0.05 and *** p<0.01.
Conclusions
The current and future viability of the U.S. health care system rests on the adequacy and reliability of the industry’s pool of primary care professionals. However, given the impending shortages of primary care physicians, the industry must look at nurse practitioners as alternative providers of primary care services. This study’s results contend that extending nurse practitioners’ professional independence could actually encourage them to allocate their working time to administration and consultation at the expense of reduced time for direct patient care. Even though the work time allocation result could draw some valuable work time away from their initial work priority (or expectation) of providing regular patient care services, it nonetheless could prominently increase the overall health care access and welfare of patients.
The results of the event study analysis indicate that the impact of full SOP laws is not temporary but persists for years after adoption. Its long-lasting impact on labor supply dynamics among nurse practitioners could improve the landscape of the health care market in the long run. Moreover, full SOP laws substantially benefit people in rural areas and those with pressing medical care needs.
This study also provides evidence on migratory patterns arising from different policy environments affecting professional independence. This study’s results do not indicate significant emigration tendencies among attract nurse practitioners working in restrictive states. However, the labor supply of nurse practitioners in full SOP states will increase because registered nurses, particularly those with higher skills and ability credentials, become more likely to pursue further studies and become nurse practitioners in the future. The findings of increased enrollment in advanced practice nurse programs support the expected full SOP law effect: both the number and productivity of health care workers increase.
However, our findings also have implications for several important areas of health care delivery that may need the attention of policymakers as they formulate and adopt SOP laws. First, professional independence grants nurse practitioners the freedom to prioritize their choices among alternative functions. We argue that the increased working time devoted to administration and consultation may improve healthcare access but nonetheless would still cite that such work emphasis could possibly shift work time away from direct patient care responsibilities.5This concern, however, can be assuaged by this study’s findings that there is significantly higher overall work-time allocation in a full SOP environment, which ensures increased attention to patients’ general needs. This effect would reduce the law’s effectiveness in expanding patients’ direct health benefits and enjoyment of essential, crucial medical attention. Thus, the government and other nursing regulatory bodies must deliberately devise incentive schemes that can prod independent practice nurse practitioners to accommodate direct patient care services in their time allocation decisions.
Second, this study’s findings on nurse practitioners’ shift to ambulatory care services while reducing their time commitment in community health centers (though not statistically significant by empirical analysis) should also warrant attention. Community health centers are widely believed to play a crucial role in delivering primary care to the underserved populations in the U.S. (Shi and Stevens 2007; Rust et al. 2009; Hawkins and Groves 2011). The diminished presence and involvement of nurse practitioners in these agencies may adversely affect health care access in underserved communities.
Third, we recognize a limitation of this study concerning the lack of relevant information on labor productivity levels of nurse practitioners after full SOP law adoption. Poghosyan, Boyd, and Knutson (2014) provide suggestive evidence showing a possible link between full SOP laws and improved teamwork among nurse practitioners. Moreover, less restrictive practice environments could also increase the marginal productivity of health care workers (Markowitz et al. 2017). This study finds a stable trend in the wage levels of nurse practitioners that could result possibly from labor supply and demand adjustments in the health care market. However, such trend could also be partly attributed to the relatively consistent productivity levels of nurse practitioners over time. Further studies can explore possible relationships between full SOP law adoption and trends in collaboration and teamwork between nurse practitioners and other health professionals, such as physicians, registered nurses, and physician assistants.
Professional autonomy for nurse practitioners would promote a more efficient allocation of the health labor force and enable nurse practitioners to utilize fully their acquired knowledge and training. These positive improvements will translate to patients’ increased health care access and better health status while nurse practitioners gain extra job fulfillment from realizing their optimal potentials.
References
Adams, E. K., & Markowitz, S. (2018). Improving efficiency in the health-care system: Removing anticompetitive barriers for advanced practice registered nurses and physician assistants. Brookings Institution. The Hamilton Project: Policy Proposal: 8.
American Association of Nurse Practitioners. (2020). NP Fact Sheet. https://www.aanp.org/about/all- about-nps/np-fact-sheet
Angrist, J. D., & Pischke, J. S. (2008). Mostly harmless econometrics: An empiricist’s companion. Prince- ton university press.
Barnes, H., Richards, M. R., McHugh, M. D., & Martsolf, G. (2018). Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Affairs, 37(6), 908–914.
Borjas, G. J., Grogger, J., & Hanson, G. H. (2008). Imperfect substitution between immigrants and natives: a reappraisal (No. w13887). National Bureau of Economic Research.
Bureau of Labor Statistics, U.S. Department of Labor. Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners. Occupational Outlook Handbook. Available at https://www.bls.gov/ooh/healthcare/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm (visited September 09, 2020).
Chetty, U. J., O’Donnell, P., Blane, D., & Willems, S. (2016). The role of primary care in improving health equity: report of a workshop held by the WONCA Health Equity Special Interest Group at the 2015 WONCA Europe Conference in Istanbul, Turkey. International journal for equity in health, 15(1), 128.
Cai, J., & Kleiner, M. (2016). The Labor Market Consequences of Regulating Similar Occupations: The Licensing of Occupational and Physical Therapists. Upjohn Institute Working Papers, 16-259, Available at SSRN: https://ssrn.com/abstract=2802158 or http://dx.doi.org/10.2139/ssrn.2802158.
DeAngelis, C. D. (1994). Nurse practitioner redux. Journal of the American Medical Association, 271(11), 868–871.
Dierick‐van Daele, A. T., Metsemakers, J. F., Derckx, E. W., Spreeuwenberg, C., & Vrijhoef, H. J. (2009). Nurse practitioners substituting for general practitioners: randomized controlled trial. Journal of advanced nursing, 65(2), 391–401.
Dueker, M. J., Jacox, A. K., Kalist, D. E., & Spurr, S. J. (2005). The practice boundaries of advanced practice nurses: an economic and legal analysis. Journal of Regulatory Economics, 27(3), 309-330.
Grumbach, K., Hart, L. G., Mertz, E., Coffman, J., & Palazzo, L. (2003). Who is caring for the under-served? A comparison of primary care physicians and nonphysician clinicians in California and Washington. Annals of Family Medicine, 1(2), 97–104.
Hawkins, D., & Groves, D. (2011). The future role of community health centers in a changing health care landscape. The Journal of Ambulatory Care Management, 34(1), 90–99.
Hooker, R. S., & McCaig, L. F. (2001). Use of physician assistants and nurse practitioners in primary care, 1995–1999. Health Affairs, 20(4), 231–238.
Kalist, D. E., & Spurr, S. J. (2004). The effect of state laws on the supply of advanced practice nurses. International Journal of Health Care Finance and Economics, 4(4), 271–281.
Kinnersley, P., Anderson, E., Parry, K., Clement, J., Archard, L., Turton, P., … & Rogers, C. (2000). Randomised controlled trial of nurse practitioner versus general practitioner care for patients requesting “same day” consultations in primary care. BMJ, 320(7241), 1043–1048.
Kleiner, M. M., Marier, A., Park, K. W., & Wing, C. (2016). Relaxing occupational licensing requirements: Analyzing wages and prices for a medical service. The Journal of Law and Economics, 59(2), 261–291.
Kurtzman, E. T., Barnow, B. S., Johnson, J. E., Simmens, S. J., Infeld, D. L., & Mullan, F. (2017). Does the regulatory environment affect nurse practitioners’ patterns of practice or quality of care in health centers? Health services research, 52, 437–458.
Lin, S. X., Gebbie, K. M., Fullilove, R. E., & Arons, R. R. (2004). Do nurse practitioners make a difference in provision of health counseling in hospital outpatient departments? Journal of the American Academy of Nurse Practitioners, 16(10), 462–466.
Markowitz, S., Adams, E. K., Lewitt, M. J., & Dunlop, A. L. (2017). Competitive effects of scope of practice restrictions: Public health or public harm?. Journal of health economics, 55, 201-218.
Martin-Misener, R., Harbman, P., Donald, F., Reid, K., Kilpatrick, K., Carter, N., … & DiCenso, A. (2015). Cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: Systematic review. BMJ Open, 5(6), e007167.
Martsolf, G., & Kandrack, R. (2017). The impact of establishing a full scope of practice for advanced practice registered nurses in the state of Indiana. RAND.
McMichael, B. J. (2018). Beyond Physicians: The Effect of Licensing and Liability Laws on the Supply of Nurse Practitioners and Physician Assistants. Journal of Empirical Legal Studies, 15(4), 732–771.
Meit, M., Knudson, A., Gilbert, T., Yu, A. T. C., Tanenbaum, E., Ormson, E., & Popat, S. (2014). The 2014 update of the rural-urban chartbook. Bethesda, MD: Rural Health Reform Policy Research Center.
Moody, N. B., Smith, P. L., & Glenn, L. L. (1999). Client characteristics and practice patterns of nurse practitioners and physicians. Nurse Practitioner, 24(3), 94–96.
Mundinger, M. O., Kane, R. L., Lenz, E. R., Totten, A. M., Tsai, W. Y., Cleary, P. D., … & Shelanski, M. 68. (2000). Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA, 283(1), 59–68.
National Association of Clinical Nurse Specialists. (2020). Scope of Practice. https://nacns.org/advocacy-policy/policies-affecting-cnss/scope-of-practice/. Retrieved on Oct 17th 2020.
Newhouse RP, Stanik-Hutt J, White KM, Johantgen M, Bass EB, Zangaro G, Wilson RF, Fountain L, Steinwachs DM, Heindel L, Weiner JP. (2011). Advanced practice nurse outcomes 1990-2008: a systematic review. Nursing Economic$, 29(5): 230-250.
Ortiz, J., Hofler, R., Bushy, A., Lin, Y. L., Khanijahani, A., & Bitney, A. (2018, June). Impact of nurse practitioner practice regulations on rural population health outcomes. In Healthcare (Vol. 6, No. 2, p. 65). Multidisciplinary Digital Publishing Institute.
Petterson, S. M., Liaw, W. R., Phillips, R. L., Rabin, D. L., Meyers, D. S., & Bazemore, A. W. (2012). Projecting US primary care physician workforce needs: 2010-2025. The Annals of Family Medicine, 10(6), 503-509.
Poghosyan, L., Boyd, D., & Knutson, A. R. (2014). Nurse practitioner role, independent practice, and teamwork in primary care. Journal for Nurse Practitioners, 10(7), 472–479.
Rondinelli, J. L., Omery, A. K., Crawford, C. L., & Johnson, J. A. (2014). Self-reported activities and out-comes of ambulatory care staff registered nurses: An exploration. Permanente Journal, 18(1), e108.
Rust, G., Baltrus, P., Ye, J., Daniels, E., Quarshie, A., Boumbulian, P., & Strothers, H. (2009). Presence of a community health center and uninsured emergency department visit rates in rural counties. Journal of Rural Health, 25(1), 8–16.
Sass, T. R., & Nichols, M. W. (1996). Scope-of-practice regulation: physician control and the wages of non-physician health-care professionals. Journal of Regulatory Economics, 9(1), 61-81.
Shi, L., & Stevens, G. D. (2007). The role of community health centers in delivering primary care to the underserved: experiences of the uninsured and Medicaid insured. Journal of Ambulatory Care Management, 30(2), 159–170.
Shin, P., Rosenbaum, S. J., Bruen, B. K., Lu, A., Arguello, R., & Tolbert, J. (2012). Medicaid and community health centers: The relationship between coverage for adults and primary care capacity in medically underserved communities. Kaiser Foundation Issue Paper #8293. Retrieved https://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?article=1178&context=sphhs_policy_facpubs.
Solon, G., Haider, S. J., & Wooldridge, J. M. (2015). What are we weighting for? Journal of Human Resources, 50(2), 301–316.
Sonenberg, A., & Knepper, H. J. (2017). Considering disparities: How do nurse practitioner regulatory policies, access to care, and health outcomes vary across four states? Nursing Outlook, 65(2), 143– 153.
Stange, K. (2014). How does provider supply and regulation influence health care markets? Evidence from nurse practitioners and physician assistants. Journal of Health Economics, 33, 1–27.
Timmons, E., Hockenberry, J., & Durrance, C. (2016). More Battles among Licensed Occupations: Estimating the Effects of Scope of Practice and Direct Access on the Chiropractic, Physical Therapist, and Physician Labor Market. Mercatus Research. Available at SSRN: https://ssrn.com/abstract=2845058.
Traczynski, J., & Udalova, V. (2018). Nurse practitioner independence, health care utilization, and health outcomes. Journal of health economics, 58, 90-109.
Xue, Y., Kannan, V., Greener, E., Smith, J. A., Brasch, J., Johnson, B. A., & Spetz, J. (2018). Full scope-of-practice regulation is associated with higher supply of nurse practitioners in rural and primary care health professional shortage counties. Journal of Nursing Regulation, 8(4), 5–13.
U.S. Department of Health and Human Services, & Health Resources and Services Administration. (2010). The registered nurse population. Findings from the 2008 National Sample Survey of Registered Nurses. Retrieved from http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf.
Yang, B. K., Johantgen, M. E., Trinkoff, A. M., Idzik, S. R., Wince, J., & Tomlinson, C. (2020). State Nurse Practitioner Practice Regulations and US Health Care Delivery Outcomes: A Systematic Review. Medical Care Research and Review, 1077558719901216.